The DUTCH Difference
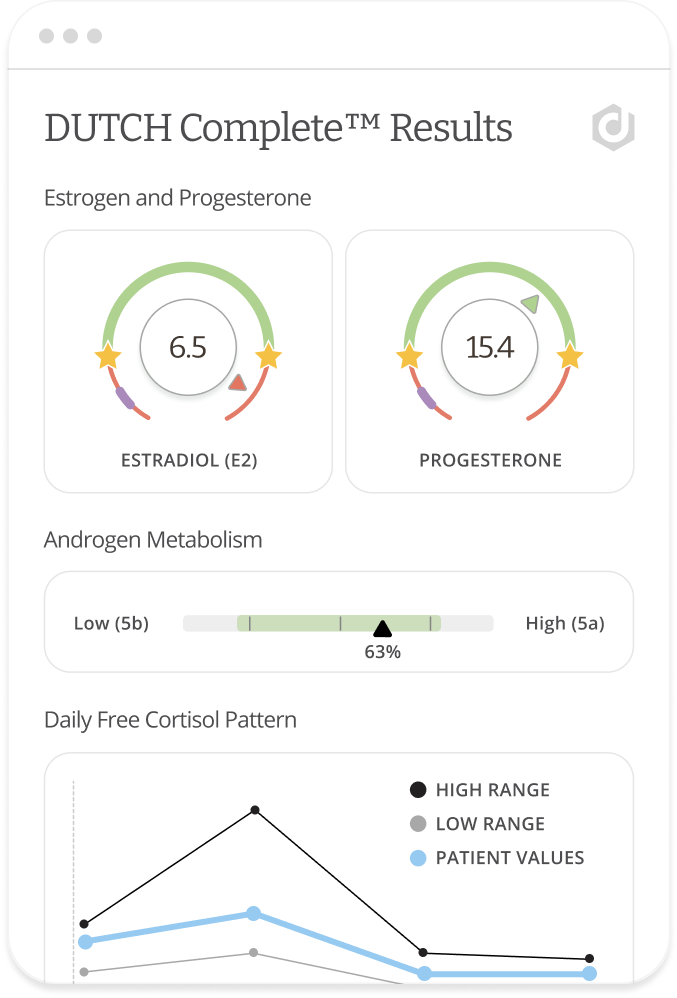
DUTCH (Dried Urine Test for Comprehensive Hormones) is a groundbreaking methodology that sets a new standard in hormone metabolite testing, surpassing traditional saliva and blood tests.
While traditional hormone diagnostics provide limited information about hormonal status, the DUTCH Test provides practitioners with a complete picture of patient hormone levels and metabolism to help solve complex clinical questions with easy at-home collection.
- Non-Invasive and Convenient
- Detailed Analysis of Hormone Balance
- Identify Root Causes
- Monitor Treatment Efficacy
- Peer-Reviewed Research
- Expert Education & Clinical Support
- Redefine Patient Outcomes
Every Sample Has a Story
DUTCH offers the most comprehensive testing for sex and adrenal hormones, along with their metabolites. This extensive data helps providers identify the root causes of symptoms, allowing for personalized treatment plans and peace of mind—all from the comfort of home.
Whether dealing with hormone-related issues like fibroids, infertility, PCOS, low testosterone, or perimenopause, or simply looking to optimize hormone health, the DUTCH Test can help deliver the insights that you need.
Support Beyond the Basics
Stay ahead in cutting-edge hormone health with personalized consultations, advanced training, and easy-to-understand resources. Our team of DUTCH clinical experts guides providers through support and education to continually improve the lives of patients.
-478WprIPxE4hwWo5K3upQZskSMcsvq.png)
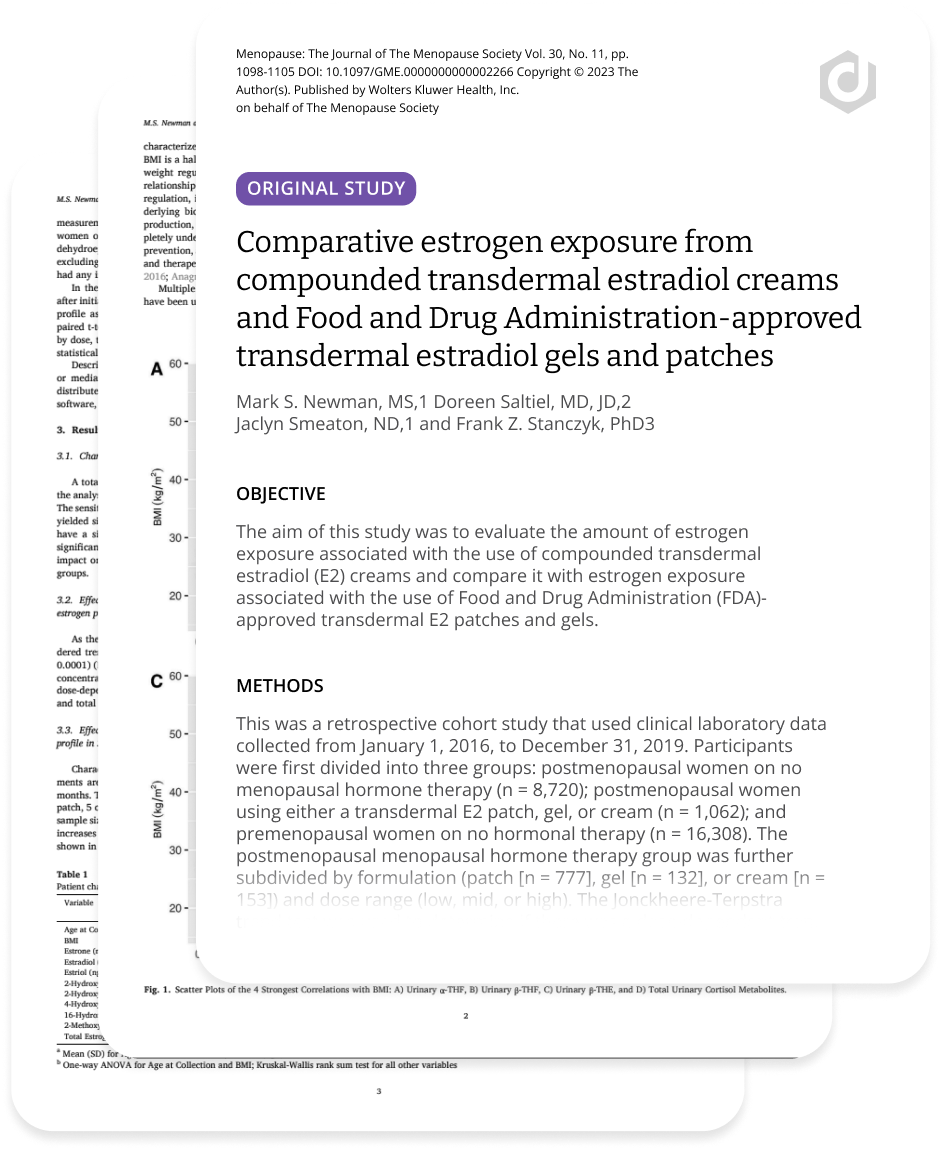
We Let the Science Speak
Our rigorous commitment to gold-standard methodologies in hormone testing has yielded multiple peer-reviewed studies validating dried urine as a reliable alternative to blood or saliva for monitoring many forms of hormone therapy. Using the most accurate method available (LC-MS/MS), our tests are trusted by thousands of providers and patients worldwide.
-5rf5SE1aTQnCOFuNgG4jPUncSnlJZy.png)
-478WprIPxE4hwWo5K3upQZskSMcsvq.png)
-5rf5SE1aTQnCOFuNgG4jPUncSnlJZy.png)
Hormone Insights for Numerous Conditions
DUTCH markers enable providers to revolutionize patient care.
Sex Hormones Panel
Adrenal Panel
Organic Acids Test (OATs) Panel
Clarity Across Diverse Patient Profiles
Providers can use information gleaned from DUTCH Markers to investigate hormonal contributions to issues including:
Actionable Results
Powered By Expert Education
We empower our providers with resources to implement DUTCH testing effectively, enabling personalized treatment plans based on industry-leading insights.
DUTCH Trust Means Rigorous, Peer-Reviewed Research
We relentlessly pursue the most accurate and precise testing techniques available.
Explore Our Research
Dive into our comprehensive collection of published and peer-reviewed research, continuously updated with the latest studies, insights, commentaries, and perspectives. Our comprehensive forum for endocrinology and metabolic research features the most current findings and advancements, ensuring providers stay well-informed.
How DUTCH Testing
Makes a Difference
Explore real-life examples from providers and patients who have benefited from using DUTCH Tests.

ND, FABNE, MPH
Carrie Jones
“The DUTCH Test allows me to help my patients see meaningful differentiation in their results, which helps me create even better treatment plans.”

MS, RD, CDN, CNS
Esther Blum
Women are suffering through perimenopause and we have to do better. Every one of my clients gets a DUTCH Complete™. It’s a great system of checks and balances. I don’t ever send someone out to get hormones until I do a DUTCH Test.

Patient
Kristen B
I will probably have a DUTCH Test once a year for as long as I’m alive, because I feel like I get a really good launching pad just to help me be the healthiest version of myself.



















