Why Assessing Progesterone Is Better with DUTCH
Mark Newman, MS
Why Assessing Progesterone Is Better with DUTCH
by Mark Newman, MS
In July of 2017, we had an excellent post from Dr. Schroeder about why we test cycling women within days 19-22 of their cycle. As many practitioners know, the mid-luteal phase is the best time to assess progesterone, a very important hormone marker for overall cycle health. Progesterone is only secreted in abundance after ovulation. Knowing whether a woman reaches healthy progesterone levels in the luteal phase is key to understanding her physical and emotional well-being, as well as her fertility.
Conventionally, serum progesterone is used to assess whether a woman has ovulated. The urine metabolites in the DUTCH test have been shown to correlate strongly to these measurements. However, in a study published in 1984[1], it was found that serum progesterone has dramatic fluctuations in the mid to late luteal phase throughout the day. The study evaluated serum progesterone and Luteinizing Hormone (LH) every 10 minutes for 24 hours in women throughout their luteal phase. This frequent sampling of the serum revealed more frequent low amplitude LH pulsations than had been previously characterized. These LH pulsations resulted in frequent fluctuations of progesterone secretion from the corpus luteum. These fluctuations were so dramatic that a woman could go from a high progesterone result to a relatively low result in a short period of time. The following graph is from the published data:
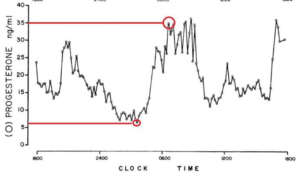
“ in the mid- and late luteal phase, plasma progesterone concentrations rapidly fluctuated during the 24-h studies from levels as low as 2.3 to peaks of 40.1 ng/ml, often within the course of minutes.”[1]
In fact, the researchers along with conventional medical professionals have concluded that when a single luteal phase serum progesterone is low, the result is considered inconclusive rather than diagnostic of a luteal phase defect or lack of ovulation. Since only low results would trigger therapy considerations, it is not ideal to base any therapy on a single serum result. If providers were able to measure serum several times throughout the day and average the results, clinical decisions could be made with more confidence. This is conceptually what the DUTCH test allows you to do, with simple urine collections.
How is urine testing different? And how is the DUTCH test better?
Urine tests reflect an average of the hours prior to the test rather than a single moment because urine fills the bladder usually over a period of 1-2 hours or longer. With serum (and saliva) we see a sampling of the current hormone levels. In other words, if you happen to catch her when she’s in the luteal phase, you can conclude she ovulated, but if you happen to catch her in a low point, it may be more ambiguous.
With urinary progesterone metabolites , the result reflects an average of her hormone production since her last urination. If you look at the graph above, you’ll see that a single urine result is an improvement on a single serum result because it covers a longer span of time. Progesterone gets metabolized primarily down two pathways, creating a 5a-pregnanediol and 5b-pregnanediol metabolite. Both metabolites have been shown to correlate to serum values.
For our cycle mapping report, we have women collect their samples first thing in the morning, which typically represents the longest span of time a person goes without urinating. This single collection is very useful in assessing progesterone production for that day.
The DUTCH Complete uses the average of 4 urine samples over the day to assess hormone production. The graph below shows the time periods we are sampling (A, B, C and D) overlaid on the graph from the 1984 study to show how progesterone activity throughout the day is assessed more comprehensively by our test.
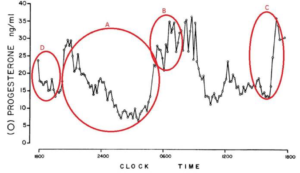
The time periods that the 4 samples for the DUTCH Complete/Plus are circled in red. A is the waking sample, B is the morning, C is the afternoon and D is the before bed sample collection.
This demonstrates how truly useful the DUTCH method is in assessing women for hormone balance and fertility. A low progesterone result on urine testing, if the timing in her cycle is correct, may be more useful in the diagnosis of luteal phase defect than a low serum result.
How is DUTCH superior to other urine tests?
It may seem redundant to test both a-pregnanediol and b-pregnanediol. It is not! There is real biochemistry going on in each woman’s body, and women have unique metabolism patterns. Each pathway (alpha and beta) represents about half of the progesterone being produced. One woman may heavily prefer the alpha pathway while another may push more heavily down the beta pathway. These two pathways are analogous to the pathway options for testosterone. Women with PCOS, for example, tend to push testosterone down the alpha pathway towards the more potent DHT. These women will also tend to push progesterone down its alpha pathway. Most labs only measure b-pregnanediol and PCOS women (who may well be progesterone deficient) would likely have their progesterone production underreported by labs only offering b-pregnanediol. Patients with hypothyroidism, on the other hand, tend to push much more heavily down the beta pathway and may be overreporting progesterone production if both progesterone pathways are not represented. Reporting both major progesterone pathways is just another way that the DUTCH test aims to provide the most accurate hormonal representation possible for you and your patients.
- Filicori, M., J.P. Butler, and W.F. Crowley, Neuroendocrine regulation of the corpus luteum in the human. Evidence for pulsatile progesterone secretion. J Clin Invest, 1984. 73 (6): p. 1638-47.
TAGS
Estrogen and Progesterone
Premenopausal Women
Laboratory Testing: In-Depth Look at DUTCH Urine Testing
Functional Laboratory Testing: General
Women's Health