Get your ticket to DUTCH Fest 2026! Join us March 12-14 in Dallas, TX for cutting-edge hormone education and hands-on learning. Learn more and register today.*
*DUTCH Fest is exclusive to registered DUTCH Providers. Only registered DUTCH Providers can attend.
Supporting Menopause with the DUTCH Test
Kaitlin Tyre, ND
Menopause marks the permanent cessation of a woman’s menstrual cycle and is triggered by the decline in ovarian hormone production—primarily estrogen and progesterone. Although menopause is a natural biological process and is not inherently classified as a disorder, the symptoms accompanying this shift can be quite impactful. Thankfully, we have methods like the DUTCH test to further analyze and understand the hormonal landscape of our patients going through this life stage. These assessments can guide personalized approaches to lifestyle, nutrition, and, when appropriate, hormone therapy to improve quality of life and long-term health outcomes for these patients.
Clinically, menopause is diagnosed after 12 consecutive months without a menstrual period. The transition into post-menopause happens gradually along a continuum that includes perimenopause, which lasts on average 2-8 years. While menopause may mark the end of a woman’s menstrual cycling career, it also marks the beginning of a new physiological hormone state that brings with it many new symptoms, clinical presentations, and health risks to consider. The sharp drop in estrogen (and progesterone) that comes with menopause can lead to common complaints such as vasomotor symptoms (VMS), which include hot flashes, night sweats, and heart palpitations, in addition to symptoms of genitourinary syndrome of menopause (GSM) such as vaginal dryness, increased frequency of UTIs, and painful sex. Brain fog, mood changes, sleep disturbance, low libido, and weight gain or weight loss resistance are other common complaints. Less common but often equally distressing symptoms include hair and skin changes associated with this new hormonal state of menopause.
If we know that estrogen and progesterone are consistently low in a postmenopausal female, why would it be helpful to evaluate postmenopausal hormones using the DUTCH test? The DUTCH test not only provides accurate insights into lower postmenopausal levels of sex hormones through “meaningful differentiation”1 and a highly sensitive and specific method of LC-MS/MS, but it can also evaluate adrenal function, nutritional and inflammatory markers, and very importantly, hormone detoxification patterns that can potentially worsen common menopausal symptoms and health outcomes.
DHEA, Cortisol, and Menopause
Assessing adrenal function through DHEA and cortisol levels may provide insight into common menopausal symptoms. DHEA functions as a master prohormone and becomes the primary source of postmenopausal androgens and estrogens. DHEA is important for energy, mood, libido, muscle mass, bone health, cardiovascular health, immune system function, among others.2 While DHEA naturally declines with age, having adequate DHEA levels during and after the menopause transition may lessen the severity of menopausal symptoms.3
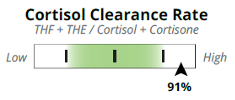
Cortisol has been shown to elevate during the late menopausal transition and into early post-menopause from the physiological impacts of menopausal hormone shifts alone4. High free cortisol and high cortisol output, the latter measured by metabolized cortisol on the DUTCH test, can exacerbate or contribute to menopause symptoms. These overlapping symptoms of high cortisol include anxiety, weight gain around the midsection, brain fog,5,6 hair loss, and sleep disturbance. Additionally with DUTCH we can assess a Cortisol Clearance Rate (CCR), which measures how well someone metabolizes their cortisol. This clearance rate can be clinically impactful because if someone does not metabolize or “clear” their cortisol well, they may experience symptoms of high cortisol. One cause for a slow CCR includes low thyroid function, which by itself can have overlapping symptoms with menopause such as brain fog, hair loss, and weight gain among others. Sluggish liver metabolism (cholestasis and NAFLD) and severely restricted caloric intake (including a history of or current anorexia) can also contribute to a sluggish CCR.7
Estrogen and Menopause
While estrogen levels are presumed to be low after menopause, there are certain cases when they may be elevated. One cause for elevated postmenopausal estrogens is increased aromatization from excess adipose or fat tissue. This elevation poses an inherent risk for endometrial cancer so ensuring that levels are within post-menopausal range with DUTCH may be a helpful preventative tactic. Additionally, even at levels within the postmenopausal range, estrogen metabolism still matters in terms of health outcomes like breast cancer.8,9 Using DUTCH to evaluate these metabolic pathways at low levels may still be helpful for this reason. Assessing baseline estrogen levels and metabolism patterns can also be a great first step when considering menopausal hormone therapy (MHT) to optimize detoxification pathways before and/or while adding bioidentical estrogen to the mix.
Progesterone and Menopause
Without ovulation, there can be no progesterone- at least no progesterone beyond what our adrenal glands can provide, which is very little. Progesterone is the first to decline in the menopausal transition and stays low after menopause. This decline can be particularly impactful for mood and sleep when we lose a-pregnanediol’s support of our calming GABA receptors. It can be helpful to evaluate progesterone metabolism if supplementing bioidentical progesterone to see if metabolism favors more a- or b-pregnanediol if seeking that calming GABA support of progesterone.
Androgens and Menopause
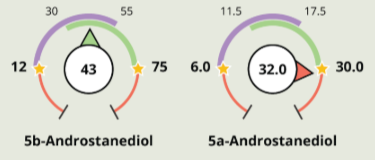
Androgens decline gradually over a lifespan but do not have a sharp drop-off like progesterone and estrogen do in menopause. This dynamic creates an inherently more androgen dominant state even if testosterone levels are not elevated. This can lead to concerning physical symptoms like acne, unwanted facial hair growth, and female pattern balding.10 In addition to evaluating testosterone (and DHEA) levels with DUTCH testing, we can gain further insight into androgen metabolism by looking at the activity of the 5a-reductase enzyme. This helps us assess androgenic metabolites like 5a-androstanediol—a downstream marker of 5a-DHT, our most potent androgen. Because 5a-DHT acts intracellularly in target tissues such as the skin, tracking its metabolites offers a more complete picture of androgen activity. If these alpha androgen metabolites are elevated, addressing relevant contributing factors like inflammation and blood sugar dysregulation may be beneficial. Other supportive strategies could include 5a-reductase inhibiting supplements such as saw palmetto, EGCG, reishi mushroom, and nettle root, among others. On the other hand, if androgens are low and metabolism favors the 5b-reductase pathway, patients may experience symptoms like low libido, poor muscle maintenance, low mood, and fatigue. In such cases, DHEA or testosterone therapy, herbal androgens like shilajit, shatavari, and damiana, as well as strength training, may be considerations to support healthier androgen levels and symptom resolution.
Menopause and the DUTCH Test
The DUTCH test is not just helpful for looking at sex and adrenal hormones but can highlight organic acids that may indicate higher levels of inflammation. Inflammation is a major driver for cardiovascular disease, which is a greater risk after menopause with the decline in estrogen and its myriad benefits on the cardiovascular system.11 Inflammatory patterns to evaluate on the DUTCH test include elevated cortisol with high CCR, high 4-OH-E1, high kynurenate, high quinolinate, and high 8OHdG. Addressing these markers and more importantly, the underlying sources of these elevated markers, may help support healthier levels of inflammation.
While the DUTCH test is helpful to evaluate and optimize endogenous postmenopausal hormones, it is additionally a great tool to monitor several types of MHT in the postmenopausal patient to maximize benefit and mitigate harm. For providers wanting to learn the up-to-date basics of using MHT in their practice, become a DUTCH Provider today to gain access to our educational course on MHT. If unsure about MHT and want to read an in-depth analysis of the WHI study that led to fear around MHT, please check out my recent article here.
References
1. Newman M. Know your lab’s reference ranges when prescribing estrogen replacement therapy. DUTCH Test. Published September 27, 2022. Accessed April 22, 2025. https://dutchtest.com/articles/know-your-labs-reference-ranges-when-prescribing-estrogen-replacement-therapy
2. Papadopoulou-Marketou N, Kassi E, Chrousos GP. Adrenal Androgens and Aging. [Updated 2023 Jan 18]. In: Feingold KR, Ahmed SF, Anawalt B, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from:
3. Samaras N, Samaras D, Frangos E, Forster A, Philippe J. A review of age-related dehydroepiandrosterone decline and its association with well-known geriatric syndromes: is treatment beneficial?. Rejuvenation Res. 2013;16(4):285-294. doi:10.1089/rej.2013.1425
4. Woods NF, Mitchell ES, Smith-Dijulio K. Cortisol levels during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women's Health Study. Menopause. 2009;16(4):708-718. doi:10.1097/gme.0b013e318198d6b2
5. de Souza-Talarico JN, Marin MF, Sindi S, Lupien SJ. Effects of stress hormones on the brain and cognition: Evidence from normal to pathological aging. Dement Neuropsychol. 2011;5(1):8-16. doi:10.1590/S1980-57642011DN05010003
6. Tatomir A, Micu C, Crivii C. The impact of stress and glucocorticoids on memory. Clujul Med. 2014;87(1):3-6. doi:10.15386/cjm.2014.8872.871.at1cm2
7. Ruef K. You need free cortisone and metabolized cortisol to evaluate HPA axis health. DUTCH Test. Published June 27, 2023. Accessed April 22, 2025. https://dutchtest.com/articles/you-need-free-cortisone-and-metabolized-cortisol-to-evaluate-hpa-axis-health
8. Fuhrman BJ, Schairer C, Gail MH, et al. Estrogen metabolism and risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 2012;104(4):326-339. doi:10.1093/jnci/djr531Falk et al.
9. Falk, R.T., Brinton, L.A., Dorgan, J.F. et al. Relationship of serum estrogens and estrogen metabolites to postmenopausal breast cancer risk: a nested case-control study. Breast Cancer Res 15, R34 (2013).
10. Zouboulis CC, Blume-Peytavi U, Kosmadaki M, et al. Skin, hair and beyond: the impact of menopause. Climacteric. 2022;25(5):434-442. doi:10.1080/13697137.2022.2050206.
11. Hyatt T. The role of estrogen, progesterone, & testosterone in heart health. DUTCH webinar. February 26, 2025. Accessed April 22, 2025. https://dutchtest.com/webinars/estrogen-progesterone-testosterone-heart-health
TAGS
Women's Health
Menopause
Adrenal Androgens (DHEA)
DHEA
Cortisol
Estrogen and Progesterone
Low Estrogen
Hormone Replacement Therapy (HRT)