Reducing the Effects of Endometriosis: How Anti-Inflammatories, Including Melatonin, May Help
by Clinical Consulting Team
This post was written by our guest author, Alana Campbell, ND, L.Ac

Endometriosis is a severely debilitating disease characterized by dysmenorrhea, pelvic pain, dyspareunia, and infertility. The true prevalence of endometriosis is largely underestimated due to the reliance on laparoscopy for diagnosis. The current estimate is 10-15% of women between the ages of 25 and 35 years old and 70% of women with chronic pelvic pain have endometriosis.1 This lack of understanding in its diagnosis and management is reflected by the fact that diagnosis is often delayed by 8-10 years after the onset of symptoms.
The effect of endometriosis goes beyond debilitating pain. The disease process changes the environment of the whole pelvic bowl, leading to chronic inflammation and adhesions in the surrounding structures. These changes have a significant effect on the health of our reproductive system and fertility. In females with infertility, it is estimated that 20-50% of them have endometriosis. In those already diagnosed with endometriosis, 35-50% of people have been diagnosed with infertility.3
Research shows the most effective treatment for advanced endometriosis is surgery, followed by suppressive therapy, which may include hormonal contraception. As endometriosis is an estrogen-dependent disease, therapies involving progesterone are beneficial. Additional progestogens have the ability to control the growth of endometriotic tissue and manage symptoms.4 However, the recurrence rate of endometriosis after surgery is extremely high, and hormonal contraceptives are not suitable or completely effective for everyone, particularly those desiring to get pregnant. It is important to explore other possible options for managing pain and disease progression.
Endometriosis is a Complex Disease
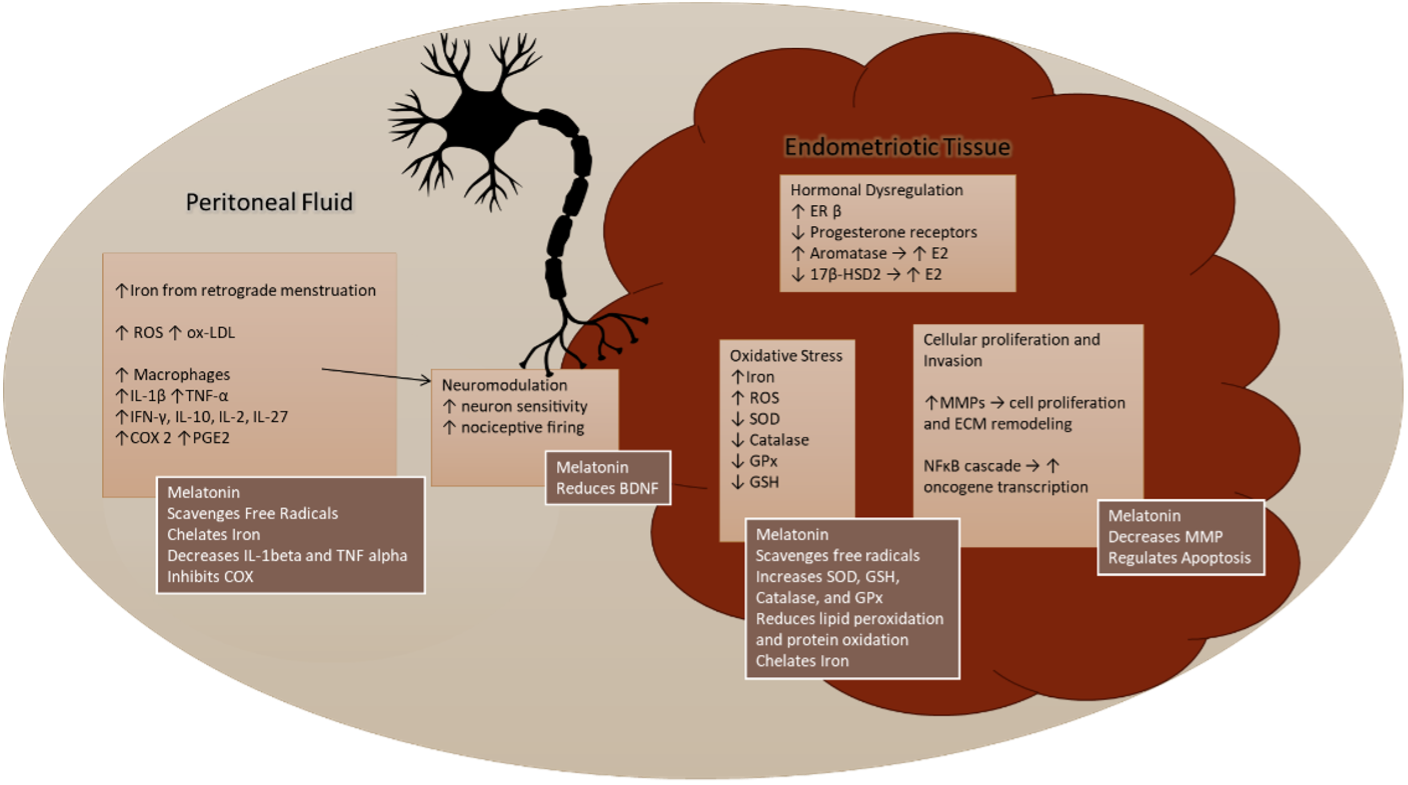
While research for this disease has been marginalized for decades, current researchers have been making strides in understanding its pathophysiology. We know that endometriosis is driven by multiple cellular factors, including hormone dysfunction, inflammation, oxidative stress, oncogenic cellular proliferation, invasion into surrounding tissues, and neuromodulation.5
Hormone Dysregulation
Endometriotic tissue has higher estradiol receptivity and lower progesterone receptivity compared to eutopic endometrium.5 There is increased aromatase, which produces estrogen, as well as decreased 17β-hydroxysteroid dehydrogenase 2 (17β-HSD2), which breaks down estradiol to estrone, a more inert form of estrogen.5 Endometriotic cells have more estrogen receptor β (ER-β), which strongly bind to estradiol and drive a vast majority of the cellular dysfunctions, like those we see in endometriosis.5 In conjunction with this increased estradiol activity, there is a downregulatory feedback loop of progesterone receptors in those tissues, which serves to protect from the negative effects of ER-β.5
Inflammation
ER β activity markedly increases interleukin-1β, a key driver in inflammation.5 The peritoneal fluid in people with endometriosis contains increased levels of inflammatory cytokines, prostaglandins, and macrophages.5 The primary players found in the endometriotic milieu are interleukin-2 (IL-2), interleukin-8 (IL-8), interleukin 10 (IL-10), interleukin-27 (IL-27), interleukin-1 β (IL-1β), interferon γ (IFN-γ), tumor necrosis factor α (TNF-α), cyclooxygenase-1 (COX-1), cyclooxygenase-2 (COX-2), and prostaglandin E2 (PGE2).5,6 All of these work in conjunction as a storm to provide the perfect setting for endometriosis to thrive: increased immune activation, macrophage infiltration, cellular proliferation, and remodeling of the extracellular matrix (ECM).6
Oxidative Stress
Dysregulated iron hemostasis also plays a significant role in endometriosis cellular changes. Retrograde menstruation, ectopic bleeding, and erythrocyte degradation lead to iron overload, which increases the cytoplasmic iron pool.6 A good amount of this cytoplasmic iron undergoes the Fenton reaction, which produces highly reactive free radicals that wreak havoc on lipids, proteins, and DNA.6 When this happens, all the intracellular antioxidants are devoted to managing these ferrous free radicals and are often unable to keep up. This leads to a buildup of reactive oxygen species (ROS), which causes apoptosis, spilling the reactive contents of the cell back into the peritoneum.6 One of those ROS, oxidized-low-density lipoprotein (ox-LDL), is highly inflammatory and recruits even more macrophages into the area.6
Neuromodulation
Chronic inflammation and oxidative stress in the peritoneum work together to modulate the nervous system and create life-altering neuropathic pelvic pain. The leukotrienes and prostaglandins promote the release of substance P and calcitonin gene-related peptide (CGRP) from the nociceptive fibers into the microenvironment.6 Prostaglandin E2 (PGE2) lowers the pain threshold in the area and increases nociceptive sensory fiber excitability.6 The ROS increase TNF-alpha receptors and increase nociceptive cation channels leading to hyperalgesia.6
Cellular Proliferation
With all of the macrophages being recruited to the sites of endometriosis, we would expect the immune system to clean up this noxious tissue. However, one of the hallmarks of endometriosis is that it evades destruction by the immune system and dodges apoptosis much like cancer does. Both cytoplasmic iron and ER β promote the NF-κB cascade which is a prominent keystone of cancer pathogenesis.5,6 The NF-κB cascade turns on oncogenic transcription leading to immune-evasive, proliferative, invasive, angiogenic, and anti-apoptotic behaviors.5 Another way that the endometriotic tissue is invasive like cancer is that it changes the ECM. Elevated ROS and IL-10 recruit the transcription of matrix metalloproteinases (MMPs) which recruit neuro-vasculature and remodel the ECM, such that we have endometriotic tissue adhering to the structures of the pelvic bowl.6
While hormonal and anti-inflammatory therapeutic targets are widely used, abundance of ROS are involved in all features of this disease progression. It is important to evaluate possible therapeutic benefits to using an antioxidant as a treatment for endometriosis.
A Powerful Antioxidant Could Be the Key
Synthesized in the pineal gland from serotonin, N acetyl-5-methoxytryptamine (Melatonin), communicates information about the cycle of daylight to the body.2 It is the conductor in the orchestra of our circadian rhythm. This master regulator goes beyond telling us when to go to sleep. Melatonin receptors are found in most of the body’s organs and tissues. This hormone is a major regulator of cellular function throughout every system. Some areas of research about melatonin show that supplementation with it offers: cerebro-protection, pulmonary protection, cancer prevention, vascular protection, reprogramming of gut microbiota, cardiovascular protection, metabolic syndrome prevention, and perinatal protection.7,8
 There is also a demonstrable effect of melatonin in the reproductive system. It is important for modulating the production and function of human gonadotropins and steroids influencing puberty, follicular genesis, and menopause.8 There is a widespread amount of melatonin receptors on our reproductive organs. Shift workers have an average of 33.8% less melatonin and a significant increase in breast and ovarian cancers.9 With melatonin’s antioxidant and regulatory effects throughout the body and reproductive system, melatonin has been a target for in-vitro and murine models of endometriosis. In this way, not only do we benefit from melatonin’s antioxidant capabilities, but it also helps balance cell proliferation, extracellular matrix remodeling, inflammation, and even neurogenic pain.5
There is also a demonstrable effect of melatonin in the reproductive system. It is important for modulating the production and function of human gonadotropins and steroids influencing puberty, follicular genesis, and menopause.8 There is a widespread amount of melatonin receptors on our reproductive organs. Shift workers have an average of 33.8% less melatonin and a significant increase in breast and ovarian cancers.9 With melatonin’s antioxidant and regulatory effects throughout the body and reproductive system, melatonin has been a target for in-vitro and murine models of endometriosis. In this way, not only do we benefit from melatonin’s antioxidant capabilities, but it also helps balance cell proliferation, extracellular matrix remodeling, inflammation, and even neurogenic pain.5
As an antioxidant, melatonin and its metabolites directly scavenge free radicals.8 It also initiates a powerful antioxidant torrent, increasing expression of superoxide dismutase (SOD), glutathione (GSH), catalase, and glutathione peroxidase (GPx).8 On top of all of that, it is a metal chelator and binds to iron, preventing all the havoc those ferrous free radicals may cause.8 By bringing the balance of free radicals and antioxidants back into harmony, we get pointedly improved cellular repair and function.
Melatonin has also been shown to have anti-inflammatory and analgesic properties. It reduces inflammation by downregulating IL-1β and tumor necrosis factor α (TNF-α).8 The analgesic effect occurs through its ability to inhibit COX-2 which stimulates prostaglandin production.5,8
Lastly, melatonin can manage the unchecked cellular growth seen in endometriosis. In murine models, melatonin promotes apoptosis of endometriotic cells by increasing Bax and caspase-9 induction while reducing Bcl-2 expression.10 Furthermore, melatonin decreases MMPs which not only control cellular proliferation but also ECM remodeling.10 In this way, melatonin reverses unfavorable cellular changes, causing a regression of endometriotic foci. This effect is greater than with the aromatase inhibitor, Letrozole, in murine models.11
How can this help us treat the symptoms of endometriosis?
While the potential for the use of melatonin to treat endometriosis is promising, there are limited current clinical studies. One of the most notable randomized controlled trials looked at melatonin supplementation of 10mg over two months for people with endometriosis-associated chronic pelvic pain. The results of this study showed a reduction in daily pain scores by 39.80% and a reduction in dysmenorrhea by 38.01%.12 Levels of BDNF, a modulator of neuropathic pain, were measured and found to be significantly reduced.12 Another study looked at 5mg of melatonin nightly in people with endometriosis-associated chronic pelvic pain. The results showed that after 8 weeks, there was a significant reduction in pain scores accompanied by a reduction in analgesic use.13
Other Anti-Inflammatories That Can Help
There has been more emphasis put into studies looking at the role of other anti-inflammatories and antioxidants in endometriosis. A few important nutrients to note include curcumin, epigallocatechin-3-gallate (EGCG), resveratrol, N-acetyl-L-cystine (NAC), palmitoyl ethanolamide (PEA), vitamin E, and vitamin C.
Curcumin is widely used for pain reduction in inflammatory disorders. While there are not any clinical studies looking at curcumin use in endometriosis-related symptom management, in vitro and animal studies show potential. These studies have found that curcumin can modulate estrogen activity, decrease inflammatory cytokines, and reduce the progression of endometriosis in animal models.14
Epigallocatechin-3-gallate (EGCG), one of the major active constituents in green tea, is an important natural therapy for reproductive health. In endometriotic cellular studies, it reduces the activity of VEGF through multiple pathways as well as modulates the NFκB pathway to prevent unchecked growth.15 Additionally, in animal models of endometriotic lesions, it decreases fibrotic pathogenesis through the induction of transforming growth factor (TGF)-β1 stimulated activation of mitogen-activated protein kinase (MAPK) and Smad signaling pathways.16
 Resveratrol, another powerful antioxidant found in grapes and wine, has a good amount of research proposing its salutogenic effect in endometriosis. In vitro and in vivo studies demonstrate its ability to reduce vascularization and cell proliferation in endometrial cells by reducing VEGF and MMPs and modulating TNF-α activity.14 It has been demonstrated to modulate the activity of E2 in the endometrium, potentially reducing estrogen-endorsed endometrial proliferation.17 Furthermore, it has been studied in humans, especially in conjunction with combined oral contraceptive pills (OCPs). In one study looking at resveratrol with OCPs, aromatase and COX-2 expression was reduced in the endometrium compared to the control group.18 Another study found a significant reduction in pain, with 82% having complete resolution of pain, after 2 months of taking 30mg of resveratrol with OCPs.18
Resveratrol, another powerful antioxidant found in grapes and wine, has a good amount of research proposing its salutogenic effect in endometriosis. In vitro and in vivo studies demonstrate its ability to reduce vascularization and cell proliferation in endometrial cells by reducing VEGF and MMPs and modulating TNF-α activity.14 It has been demonstrated to modulate the activity of E2 in the endometrium, potentially reducing estrogen-endorsed endometrial proliferation.17 Furthermore, it has been studied in humans, especially in conjunction with combined oral contraceptive pills (OCPs). In one study looking at resveratrol with OCPs, aromatase and COX-2 expression was reduced in the endometrium compared to the control group.18 Another study found a significant reduction in pain, with 82% having complete resolution of pain, after 2 months of taking 30mg of resveratrol with OCPs.18
Another fantastic food-based nutrient, found especially high in garlic and onions, has been evaluated in human trials for the treatment of endometriosis. N-acetyl-L-cystine (NAC) has been demonstrated clinically to reduce dysmenorrhea, dyspareunia, chronic pelvic pain, and the use of analgesic medications at a dose of 600mg 3 times per day for 3 consecutive days of the week for 3 months.19 Furthermore, this study demonstrated a significant reduction in endometrioma size and improvement in pregnancy outcomes.19 Out of the 42 patients desiring pregnancy, 39 were successfully pregnant within 6 months of supplementation.19 The proposed mechanism of action for NAC highlights its multifactorial effect on endometriosis pathogenesis. It is an antioxidant and precursor to glutathione.19 NAC has been shown to decrease endometrial lesion size in animal studies as well as reduce TNF-alpha and COX-2 concentrations.18 This reduction of COX-2 leads to decreased levels of inflammation. Less COX-2 also means less PGE2, which stimulates aromatase, resulting in overall decreased levels of estrogen in the peritoneal fluid.14
Palmitoyl ethanolamide (PEA), an anti-inflammatory fatty acid, could be a promising nutrient in controlling chronic pelvic pain in endometriosis. PEA has been shown to have significant modulating effects on mast cells.20 The production of neurogenic pain, as seen in endometriosis, is largely mediated by mast cell activity.21 The clinical efficacy of PEA has been demonstrated in a study of 30 women taking 600mg of ultramicronized-palmitoylethanolamide (um-PEA) twice daily followed by co-micronized palmitoylethanolamide/polydatin (m(PEA/PLD)) (440mg+40mg) micro granules twice daily for 80 days. This treatment showed a significant reduction in pain and improvement in quality-of-life factors.20
Vitamin C and vitamin E both directly intervene with ROS production.14 There is a promising amount of research looking at the clinical efficacy of their use together for endometriosis. One systematic review and meta-analysis looked at doses around 1200mg of vitamin E and 1000mg of vitamin C and found a significant reduction in endometriosis-associated chronic pelvic pain, dysmenorrhea, and dyspareunia.22
In conclusion, endometriosis is a condition that goes beyond painful periods and needs to be treated as such. While therapies involving hormone and pain management can be helpful, it is not enough. The progression of endometriosis is dependent on oxidative stress and proinflammatory activation, which causes tissue destruction and infertility. There are many therapeutic nutrients that have the potential to treat endometriosis. Out of all of these, melatonin is a promising therapeutic that needs more attention in clinical trials. This natural product is highly effective in not only offsetting oxidative stress but also reducing the invasive nature of this disease.