Get your ticket to DUTCH Fest 2026! Join us March 12-14 in Dallas, TX for cutting-edge hormone education and hands-on learning. Learn more and register today.*
*DUTCH Fest is exclusive to registered DUTCH Providers. Only registered DUTCH Providers can attend.
Estrogen Tutorial
Mark Newman, MS
Estrogen Tutorial
Female Reproductive Hormones (progesterone and estrogen) & The Menstrual Cycle
The basics of the menstrual cycle
The menstrual cycle is divided up into three sections. When a woman starts her period (day 1) until she ovulates, this is known as the “Follicular Phase.” The “Ovulation Phase” typically occurs in the middle of her cycle. This is when her body is triggered to release an egg subsequently producing progesterone. Once a woman ovulates, she enters into the “Luteal Phase” until she becomes pregnant or her period starts. Typically it is during the middle of this luteal phase that samples are collected, so that proper production of both progesterone and estrogen can be made.
Declining estrogen at the end of her cycle and during bleeding stimulates her FSH (follicle stimulating hormone). FSH stimulates follicles in the ovary to grow. The growing follicles produce estrogen causing estrogen to increase again. This increasing estrogen tells the uterus to prepare itself for potential implanation, changes the cervical mucus to be more fertile, softens and opens the os of the cervix to allow potential sperm to come through. Estrogen also tells the brain to choose a main follicle that will release an egg.
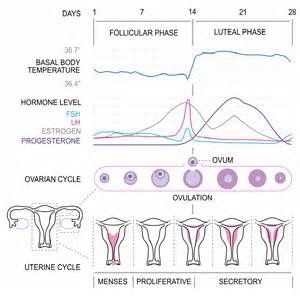
Typically around day 14-ish (but not always), estrogen surges causing LH (lutenizing hormone) to surge as well. The LH surge causes the egg to release (ovulation) about 18-36 hours later. The left over egg-less follicle is called the corpus luteum and it begins to make progesterone. This rise in progesterone causes the body temperature to increase as progesterone is ‘warming.’ A healthy luteal phase is between 12-16 days. A deficient luteal phase is under 12 days. If a woman becomes pregnant, the corpus luteum will continue to make progesterone until the placenta can take over which is around week 10. If she does not become pregnant (no implantation signals sent to the brain) then the process folds down, the hormones decline, and the lining of the uterus begins shed off and bleed.
What is the difference between pre-menopausal, peri-menopausal, and post-menopausal?
Pre-menopausal describes the time in a woman’s life when she still cycles on a regular basis. This occurs most commonly between her teen years up into her 40’s and sometimes 50’s.
Peri-menopausal describes the time prior to menopause where her hormones are starting to shift due to the ovaries beginning the process of shutting down and not cycling every month. She may experience a change in her cycle (no cycles, short cycles, long cycles, and irregular cycles) that had not been normal to her. She may also experience common symptoms such as insomnia, hot flashes, night sweats, brain fog, weight gain, joint pain, and vaginal dryness. This occurs most commonly between the 40’s and 50’s.
Once a woman has not had a period in 12 consecutive months, she is considered post-menopausal . She may still continue to have unpleasant hormonal symptoms, but she does not cycle anymore.
What if I use the birth control pill/patch/ring/implants (not IUD)?
The birth control pill (patch, ring and implants) stops the FSH and LH surge from the pituitary to prevent an estrogen rise and ovulation (thus progesterone production) from the ovary. If you hormone test while on the pill, your estrogen and progesterone should be quite low. That means the pill is doing its job and you are not likely to become pregnant.
Stopping your pill on day 19-22 will not induce ovulation AND it WILL likely bring on an early menstrual cycle or increase your risk of becoming pregnant. We do not recommend stopping the pill for a few days just to test her hormones.
Testing during the sugar pill week when you have your withdrawal period will also result in very low estrogen and progesterone numbers.
If you want to stop the pill (patch, ring or implant) and test your hormones, we encourage you have 3 full menstrual cycles without any pill, patch, ring or implant use before testing to ensure the hypothalamic-pituitary communication with the ovary is back on track as best as it can be. Make sure you use alternative methods to prevent pregnancy such as condoms!
If you are on hormonal birth control to prevent or decrease symptoms of certain conditions such as endometriosis or heavy bleeding, talk with your health care provider first before just stopping your birth control. If you stop your birth control you symptoms will likely return immediately.
What if I have an IUD?
The copper IUD also known as the Paragard is not made up of any hormones therefore you can test on the typical day 19, 20 or 21 of a 28-ish day cycle as the instructions request.
The Mirena IUD does have synthetic progesterone in it known as a progestin. For those women who still have a cycle with the Mirena, it can partially suppress ovulation in some women which will make progesterone levels sub-optimal or outright low. The progestin in the Mirena often makes the lining of the uterus very thin to almost non-existent. As a result some women do not bleed when it’s time to have their period. This can make it difficult to determine exactly what day of their cycle they are on. Please call the lab to discuss your options if you are doing sex hormones as part of your testing. If you are just doing only the adrenal test, you can collect as instructed by your health care provider.
What if I am on HRT or hormone replacement?
You are still able to use DUTCH testing when on HRT. We strongly encourage you to visit our free video library, find the route of administration you are taking (ie. oral, topical, vaginal) and watch the video in order to determine your specifics.
Estrogen
The basics of estrogens
Estrogen is made primarily in the ovaries of cycling women while smaller amounts can be converted from testosterone through a process called aromatization. In menopause estrogen production shifts almost completely to aromatization. Men need far less estrogen than women and it is aromatized in primarily from testosterone. The enzyme responsible for aromatization is found in fat tissue, the brain, gonads, blood vessels, skin, and bone.
Women who are still cycling have much greater quantities of estradiol than men, but it is important to note that men do make estrogen. In fact, the level of estrogen in men is actually higher than the level in a post-menopausal woman! The main and most potent estrogen is known as Estradiol (E2). It is made primarily in the ovaries or testes but also the fat, liver, and neural tissue. Estrone (E1) is also made by the ovary but in fat tissue in lesser quantities. While not as abundant in circulation as estradiol, estrone excess can still increase the risk for estrogen dominant cancers as well as estrogen dominant symptoms such as breast tenderness, heavy menstrual cycles, headaches, and erectile dysfunction and breast development in men just like estradiol. Estrone is commonly thought to be more abundant during menopause. Estradiol and estrone can interconvert into each other. The third estrogen is known as estriol (E3) and is produced in significant amounts during pregnancy. In men and women, Estriol is irreversibly produced by estradiol (estriol cannot make estradiol) or from estrone through 16OH-Estrone which makes it the largest circulating estrogen because both Estrone and Estradiol can make it. Despite this, estriol is not nearly as potent as estradiol (Estradiol is 80x more potent!).
The metabolism of estrogen in men and women
When looking at a DUTCH test or through this website, you may notice the word “metabolites” or “metabolized” used fairly often. When you make a hormone such as estrogen or cortisol, or when someone takes a hormone (such as in HRT), it must be processed by the body in the liver through the process of phase 1 and phase 2 detoxification before it can be excreted out the other end. This is known as hormone metabolism. As a hormone is undergoing that process, it gets changed into other forms known as metabolites.
Phase 1 Metabolism:
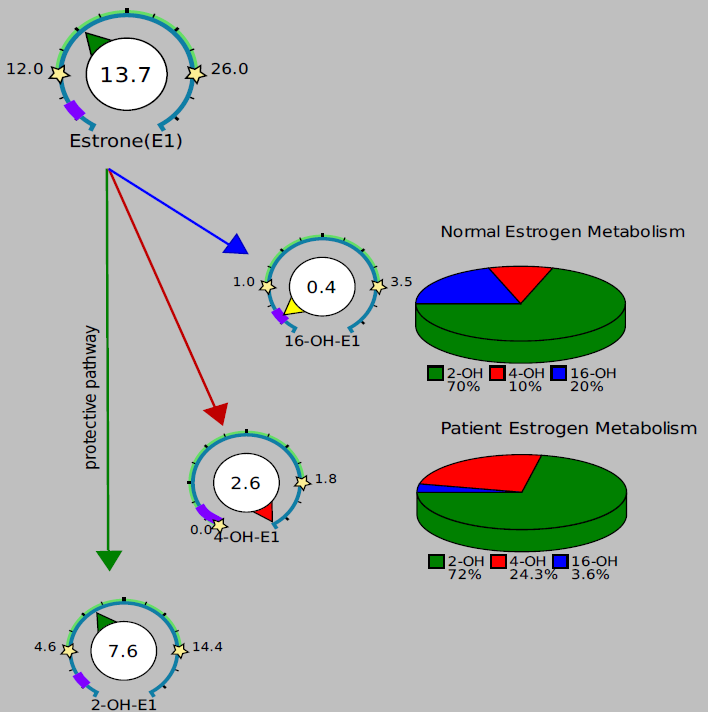
In the liver, estrone and estradiol are converted into the phase 1 metabolites known as 2OH-E1, 4OH-E1 or 16OH-E1. These metabolites can go back out into circulation before going through phase 2 detoxification where they are then excreted out of the body. The phase 1 metabolites can be more damaging to the body by causing estrogen dominant symptoms or increasing the risk for cancer in both men and women. Generally speaking, the 2OH-E1 is considered the safer metabolites as it only weakly induces cell proliferation and might even inhibit it, the 4OH-E1 can damage DNA and may be more cancer inducing.
You can assess phase 1 metabolism by looking at the relative amounts of these hormones. The top pie chart shows the three-way ratio that is typically seen. 70% of the total of the three (2OH-E1 + 4OH-E1 + 16OH-E1) usually makes up the 2OH-E1 fraction while 10% comes from the 4OH-E1 and 20% from 16OH-E1. In the example below, the 4OH-E1 pathway seems to be favored more than usual while the 16OH-E1 pathway shows much less hormone.
Phase 2 Metabolism (Methylation):
After estrogens goes through phase 1 detoxification, they move on to methylation which is part of phase 2 detoxification and reported on the DUTCH test as the Methylation Activity fan gauge. Methylation, in essence, “neutralizes” the phase 1 metabolites and prepares them to be excreted out the body instead of shuttling them back into circulation. Only 2OH and 4OH estrogens are methylated. 16OH-E1 is not. If someone has poor methylation, they may be at higher risk for estrogen dominance and estrogenic cancers.
It is important to note that methylation is not the only phase II option for these hormones. Technically every estrogen measured in the DUTCH profile is a Phase 2 metabolite because they only exist in urine as phase 2 conjugates like glucuronides. For example, all of the estradiol in urine is in one of three different forms of estradiol-glucuronide.
It is also important to note that methylation is an important detoxification step for catecholamines (like adrenaline) and other compounds. Compromised methylation can affect overall health in multiple ways and the methylation index on the DUTCH results can give excellent insight into overall methylation efficiency.
Poor methylation can be caused by nutrient deficiencies or genetic defects in enzymes (namely MTHFR and COMT). Magnesium and methyl donors (SAMe, B Vitamins, TMG, Choline, Folate, Methionine) are co-factors needed for methylation to work properly.
Do you report a 2OH/16OH ratio?
Coming soon.
Do you report a Progesterone to Estradiol ratio?
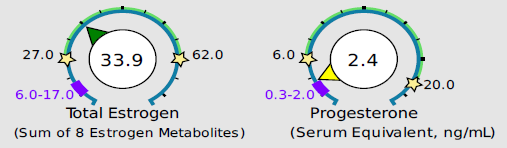
We believe that the progesterone/estradiol ratio is much more complex than simply looking at just progesterone and just estradiol. We report all 3 estrogens (E1, E2, and E3), and we evaluate estrogen’s ability to go through both phase 1 and phase 2 detoxification (methylation). We also report both the alpha and beta progesterone metabolites. This allows you to see the bigger picture as it relates to your overall progesterone levels and overall estrogen plus estrogen metabolism ability. To get an idea if someone is estrogen dominant, you can look at the arrows on the gauges for estrogen. If those levels are higher than the arrows on the progesterone gauges, then they may be estrogen dominant. Be aware though that poor estrogen metabolism may cause a person to be and feel more estrogen dominant as well and poor metabolism may be the reason someone is estrogen dominant. Again, it is important to evaluate the whole picture.
In this example, estrogens are not particularly high, but they are higher (in a relative sense) than progesterone. This patient may experience estrogen dominance symptoms even though overall estrogen levels are not exceptionally high.
Common symptoms of elevated estrogen
In women – mood swings, weight gain, breast tenderness, fibrocystic breasts, heavy menses, fibroid/polyp development.
In men – breast development, weight gain, and mood swings.
Common causes of elevated estrogen
In women – ovarian hyper-production of estrogen, PCOS, environmental/xenoestrogen exposure (this does not show up on DUTCH testing however but they can cause symptoms), moderate alcohol use (2 or more drinks per day), obesity, over aromatization from testosterone to estrogen due to inflammation and blood sugar/insulin issues
In men – over aromatization from testosterone to estrogen due to inflammation and blood sugar/insulin issues, environmental/xenoestrogen exposure (this does not show up on DUTCH testing, but they can cause symptoms), moderate alcohol use, and obesity
Common symptoms of low estrogen
In women - fatigue, depression, hot flashes, night sweats, vaginal dryness, pain with intercourse, low libido, joint pain, brain fog, migraines/headaches, fertility issues, dry skin
In men - not generally considered symptomatic, but in very extreme cases men may have similar symptoms as in the list above for women
Common causes of low estrogens in women
In women - irregular cycles, no cycles, menopause, ovarian insufficiency, removal of ovaries (ie. hysterectomy), hypothyroid, anorexia, hormonal birth control (ie. birth control pill), head trauma affecting the hypothalamus/pituitary function
Common ways to lower estrogen
Please consult with your health care provider about advice/treatment/diagnosis. The following statements are general informational statements.
In women - address the cause, avoid alcohol, avoid environmental/xenoestrogens, DIM/I3C supplementation, calcium-d-glucurate, increased fiber (especially ground flax seeds), increased detoxification support, and weight loss
In men – address the cause, avoid alcohol, avoid environmental/xenoestrogens, DIM/I3C supplementation, calcium-d-glucurate, increased fiber, decrease blood sugar and insulin, increased detoxification support, weight loss, and things that block aromatase (Chrysin, Damiana, Zinc and pharmaceutical aromatase inhibitors)
Common ways to raise estrogen
Please consult with your health care provider about advice/treatment/diagnosis. The following statements are general informational statements.
In women - address the cause, phytoestrogens such as Red Clover, Dong Quai, Kudzu, soy, diosgenin, genistein, fennel, and Black Cohosh (although studies are mixed on whether it acts as a phytoestrogen or not), Maca, and bioidentical estrogen replacement
Progesterone
The basics of Progesterone
Progesterone is made primarily in the ovaries in a cycling woman only once she has ovulated (see Menstrual Cycle section). If she does not ovulate, she will not likely make high levels of progesterone. In menopause, the menstrual cycle stops, she does not ovulate anymore and the production of progesterone falls significantly to only a small amount. The adrenal glands are responsible for making tiny amounts of progesterone too. Men need far less progesterone than women and it too is made via the adrenal glands.
Do you test progesterone?
Progesterone is not found in urine in significant amounts therefore the progesterone metabolites, a-pregnanediol and b-pregnanediol are measured instead as an indirect measurement (customary for urine testing). Extensive studies have been performed by Precision Analytical to show that these markers correlate with blood progesterone levels very well. There are also plenty of published studies showing correlation between pregnanediol and serum progesterone. The easiest way to interpret progesterone results is to assume half of the progesterone is going down the a-pregnanediol and the other half down the b-pregnanediol pathway. This is approximately true. From our impressive blood (serum) correlation data, we calculate a “serum equivalent” for progesterone. This value is reported on the first page of the DUTCH Complete and is not given on the DUTCH Sex Hormone Metabolite report.
Is it relevant if progesterone goes down one pathway more than the other?
We do not consider it highly relevant which pathway is preferred unless you are taking oral progesterone. The alpha metabolites (like a-pregnanediol) have been shown in work by John Weibe to be proliferative with in-vitro studies. In the future, there may be some relevance to the relative a-pregnanediol and b-pregnanediol values. We do believe these differences to be relevant when patients are on oral progesterone. Patients who turn oral progesterone preferentially into a-pregnanediol may make more allo-pregnanolone, which is what gives oral progesterone its sedating effects (which is why it helps you sleep).
Do you test pregnenolone? Does it show up in the DUTCH test?
The DUTCH test does not evaluate pregnenolone. This is best tested in the serum. Please be aware that taking pregnenolone supplements will likely increase the progesterone metabolites, a-pregnanediol, however it does not represent increased progesterone in the serum. Pregenolone can get metabolized itself to both a-pregnanediol and especially b-pregnanediol. This elevated level can make you think the pregnenolone is actually increasing progesterone in the body when likely is not. Our instructions ask patients to skip pregnenolone for two days before the test.
Common symptoms of elevated progesterone
Water retention, breast tenderness, headaches, mood swings
Common causes of elevated progesterone
Bioidentical progesterone supplementation, strong ovulation producing a great deal of progesterone, fertility medications
Common symptoms of low progesterone
These are the same symptoms as elevated estrogen - mood swings, weight gain, breast tenderness, fibrocystic breasts, heavy menses, fibroid/polyp development.
Common causes of low progesterone
Please consult with your health care provider about advice/treatment/diagnosis. The following statements are general informational statements.
Poor ovulation, no ovulation, irregular cycles, ovarian insufficiency, PCOS, peri-menopause and menopause, hypothalamus-pituitary-ovarian axis communication issues, hypothyroid, NSAID use (Naproxen/Aleve and Diclofenac), Mirena IUD, Accutane (isotretinoin), head trauma affecting the hypothalamus and/or pituitary function
Common ways to lower progesterone
Please consult with your health care provider about advice/treatment/diagnosis. The following statements are general informational statements.
Address the cause, reduce or eliminate progesterone supplementation, reduce or elimination progesterone supportive herbs, detoxification liver support
Common ways to raise progesterone
Please consult with your health care provider about advice/treatment/diagnosis. The following statements are general informational statements.
Address the cause, herbal support such as Chaste tree berry, Maca and Red Raspberry, vitamin B6, Evening Primrose Oil, bioidentical progesterone supplementation, Clomid
Please Note: The contents of this video are for educational and informational purposes only. The information is not to be interpreted as, or mistaken for, clinical advice. Please consult a medical professional or healthcare provider for medical advice, diagnoses, or treatment.
Disclaimer: Special offer of 50% OFF first five kits is invalid 60 days after new provider registration.
TAGS
Women's Health
Premenopausal Women
Postmenopausal Women
Estrogen and Progesterone
DUTCH Test: Basic Interpretation Resources
Estrogen Detoxification