Get your ticket to DUTCH Fest 2026! Join us March 12-14 in Dallas, TX for cutting-edge hormone education and hands-on learning. Learn more and register today.*
*DUTCH Fest is exclusive to registered DUTCH Providers. Only registered DUTCH Providers can attend.
DUTCH Complete™ Cortisol Tutorial
Mark Newman, MS
DUTCH Complete™ Cortisol Tutorial
What is free cortisol?
When the adrenal glands make cortisol, it can circulate bound up to its carrier protein (almost like a person riding on a bus) or it can circulate free (not on the bus). The most common carrier protein is called Cortisol Binding Globulin (CBG) while it binds to a lesser extent to Albumin. When a hormone is bound to its carrier protein, it does not have the ability to act. Only once it unbinds (gets off the bus) and becomes ‘free’ is it able to be active in the body. Free cortisol makes up only about 1% of the overall cortisol produced, but it is an important fraction because it is the biologically active fraction.
Cortisol typically rises quickly upon waking and then slowly drops throughout the day. The measurements of free cortisol (and to a lesser extent free cortisone) are used to assess this up-and-down pattern. While free cortisol is an important measurement, it does not necessarily reflect overall production of cortisol. The metabolites of cortisol are a better marker of cortisol production.
What is metabolized cortisol?
Metabolized cortisol is the sum of a-tetrahydrocortisol (aTHF), b-tetrahydrocortisol (bTHF), and b-tetrahydrocortisone (bTHE). They are a good indication of the total cortisol output from the adrenal gland or clearance out the body. You’ll notice these numbers are much larger than that of free cortisol because they represent a much larger fraction of the overall cortisol produced. Total adrenal gland output is important to know in comparison to the free cortisol levels. For example, if someone has low free cortisol, this does not necessarily mean their adrenal glands are not producing very much cortisol. It only means their free cortisol is low. They may have normal or high levels of total (metabolized) cortisol which is often addressed/treated differently than if someone had low free cortisol and low total (metabolized) cortisol. When free cortisol is lower (in a relative sense) than metabolized cortisol, it implies that cortisol clearance/metabolism may be higher than normal. In the following example the patient shows low levels of free cortisol even though production of cortisol is quite high (implying high cortisol metabolism/clearance).
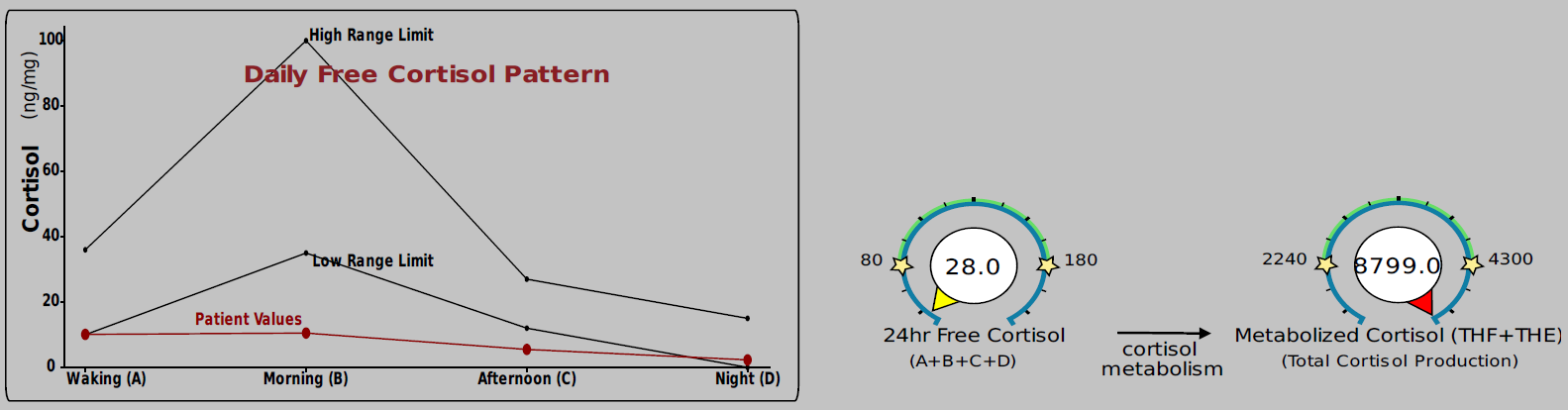
In the above example, cortisol metabolism seems to be up-regulated. In the following example, the opposite may be true.

What increases or decreases cortisol metabolism/clearance?
Cortisol and cortisone are metabolized by 5a-reductase and 5b-reductase (and then by another enzyme) to tetrahydrocortisol and tetrahydrocortisone for excretion.
This metabolism process is particularly increased (sped up) in obesity, high insulin and hyperthyroid. It may also be that long-term exposure to cortisol (long-term stress, supplementation) or other glucocorticoids speed this process up.
This metabolism process is slowed in cases of hypothyroidism, anorexia or impaired liver function.
There is also a process of metabolism where by cortisol is deactivated to cortisone (and also reactivated back to cortisol from cortisone). For the purposes of clarity, we will consider this process “deactivation” and “activation” and not “metabolism.”
What is “Hydrocortisone?”
Simply put – it IS cortisol. When you take a hydrocortisone supplement (usually a cream), you are taking active cortisol. When it is given in a cream, it tends to stay in the local area where it is applied, so you don’t get a lot of systemic exposure to cortisol unless you take a LOT. Be careful with any hydrocortisone products because if you get any on the urine collection device (or in the urine you’re collecting) it will artificially increase you values. If this happens, you’ll see cortisol go way up, but cortisone will not. In this type of case, use the cortisone value as the best approximation of your cortisol status during that time.
Cortisol → Cortisone Deactivation (11-beta-hydroxysteroid-dehydrogenase)
Cortisol can convert into its inactive form, known as Cortisone, through an enzyme known as 11bHSD-2 (located in the kidneys, saliva glands, and colon). Cortisone is not able to do all of the stress fighting or blood sugar balancing activities cortisol can do. Cortisone can be reactivated back to Cortisol if needed by a different form of the same enzyme, 11bHSD-1 (located in the liver, fat tissue, and central nervous). The balance of cortisol and cortisone metabolites best tells us which is winning out overall. You can see the gauge for this on the bottom of the DUTCH Adrenal report.

What leads to more cortisol or more cortisone?
Hypothyroidism, licorice root extract, grapefruit, inflammation, visceral obesity (belly fat), high insulin, and excess sodium can make a person lean more towards the active form cortisol.
Hyperthyroidism, human growth hormone, ketoconazole, quality sleep, magnolia, scutellaria, zizyphus, testosterone, and citrus peel extract influence the deactivation of cortisol and lead to a cortisone preference.
Why do you test the free cortisone pattern and not just cortisol?
When looking at the DUTCH Adrenal page, you will see we provide both the levels of free cortisol and free cortisone plus a graph of free cortisol and free cortisone. Cortisone is often referred to as “cortisol’s shadow.” Quite a bit of the cortisol that goes into the kidney gets quickly deactivated to cortisone (to keep cortisol from raising blood pressure). Because urine comes directly from the kidney, this local transfer is highly reflected in the urine results. As odd as it may seem, cortisone does NOT typically go up-and-down throughout the day in blood. It does in urine (this is also true of saliva) because of this local deactivation reflected heavily in urine. Because of this, cortisone provides a secondary (confirmatory) picture of the up-and-down pattern of free cortisol throughout the day. It also provides a back-up value if a sample is contaminated with cortisol (hydrocortisone) cream. For a detailed explanation of why we also test cortisone, see this post .
What if I am on a steroid medication such as prednisone, steroid inhaler, steroid allergy nasal spray or topical hydrocortisone/Cortaid cream?
As discussed prior, cortisol is also known as hydrocortisone and is a corticosteroid (meaning it comes from the cortex of the adrenal glands). Prednisone is a synthetic corticosteroid. Prednisone and other synthetic steroids (dexamethasone, triamcinolone) are much more potent and remain circulating in the body a lot longer than cortisol. They can cause a lot of side effects such as adrenal suppression, thinning skin, and weight gain however they may be necessary in an emergency or autoimmune situation. If someone is taking a steroid medication regularly, it may disrupt and suppress the adrenal gland output of cortisol resulting in very low cortisol markers on the DUTCH test.
Be aware that a “steroid hormone” and someone taking synthetic steroids such as for body building are different. When talking about body builders getting “roids” you’re talking about “anabolic steroid hormones” and cortisol is not anabolic like testosterone. “Steroid hormone” is an umbrella term for those hormones made in the cortex of the adrenal glands (ie. cortisol) or the gonads (ie. testosterone or progesterone).
There are many pharmaceutical products that contain compounds that can suppress cortisol levels. You can read more about this in this post .

*The chart indicates the type of medication on the left, the glucocorticoid power (ability to act like cortisol) mineralcorticoid power (ability to act like aldosterone), duration in the body and how strong it is compared to cortisol. Short = 8-12 hours Medium = 12-36 hours, Long = 36-72 hours
Common symptoms of elevated free cortisol
Depression, anxiety, weight gain, sleep problems, muscle weakness, thinning skin, thinning hair, high blood pressure, low sex drive, decreased sexual arousal, memory issues, and digestive issues.
Common causes of increased cortisol production by the adrenal glands
Stress (real or perceived, physical or psychological), obesity (excess adipose tissue), insulin issues, hyperthyroid, inflammation, Cushing’s disease, and HPA-axis dysfunction
Common symptoms of decreased free cortisol
Fatigue, frequent illness, joint pain, muscle pain, low blood pressure, dizziness, weakness, increased thirst, digestive issues, depression/low mood, and hypoglycemia
Common causes of decreased cortisol production by the adrenal glands
Hypothyroid, opioid medication use, corticosteroid medication use, HPA-axis dysfunction, Accutane (isotretinoin) medication use, chronic marijuana use, and head trauma affecting the function of the hypothalamus/pituitary.
What helps lower cortisol levels in the body
Please consult with your health care provider about advice/treatment/diagnosis. The following statements are general informational statements.
Address the cause of the high cortisol levels, improve sleep quality, rest, prayer/meditation, weight bearing or resistance training, lowering stress, eliminating inflammatory foods, reduce inflammation overall, weight loss, vitamin C, B-vitamins, phosphytidyl serine, HPA-axis support and herbs such as skullcap, magnolia, and zizyphus.
What helps raise cortisol levels in the body
Please consult with your health care provider about advice/treatment/diagnosis. The following statements are general informational statements.
Address the cause for the low cortisol levels, improve sleep quality, rest, vitamin C, B-vitamins, licorice root (warning: watch for high blood pressure and low potassium), glandular supplements, and HPA-axis support. Obviously taking cortisol supplementation will also increase cortisol levels. This should never be done without proper justification and a prescription from a healthcare provider.
Please Note: The contents of this video are for educational and informational purposes only. The information is not to be interpreted as, or mistaken for, clinical advice. Please consult a medical professional or healthcare provider for medical advice, diagnoses, or treatment.
Disclaimer: Special offer of 50% OFF first five kits is invalid 60 days after new provider registration.
TAGS
DUTCH Test: Basic Interpretation Resources
Cortisol
Cortisol Metabolism
Women's Health
Men's Health