Get your ticket to DUTCH Fest 2026! Join us March 12-14 in Dallas, TX for cutting-edge hormone education and hands-on learning. Learn more and register today.*
*DUTCH Fest is exclusive to registered DUTCH Providers. Only registered DUTCH Providers can attend.
Menopausal HRT Series: Can progesterone cream provide endometrial protection?
Tori Hudson, ND
Menopausal HRT Series: Can progesterone cream provide endometrial protection?
by Tori Hudson, ND
Read about progesterone creams in part 3 of our Menopausal HRT blog series. This series will focus on classic myths that can lead to depriving women of hormones they may need, prescribing insufficient doses of progesterone in combination with systemic estrogen, the subject of bioidentical hormones and compounding, and more.
Myth: Progesterone cream is an adequate delivery method to provide endometrial protection in women who take systemic estrogen.
There are very specific doses, forms, and deliveries of progestogens that are accepted methods of providing adequate endometrial protection, based on adequate studies. Five studies have been identified investigating the impact of transdermal micronized progesterone on the endometrium. All but one study were randomized controlled trials, some of which had a placebo or a progestin as a comparator. Sample sizes range from 27 to 54 postmenopausal women and study duration ranged from 4 weeks to 48 weeks. Hopefully, you can see the problem already -- studies were too small and too short to conclude safety.
The estrogens were applied either orally or transdermally, and the dosing ranges were from high end of normal dosing to moderate dose categories. The transdermal progesterone cream was applied either sequentially or continuously and ranged from 16 mg/day to 64 mg/day. In one study, a transvaginal ultrasound showed a significant increase in endometrial thickness. All five studies had an endometrial biopsy before and after treatment. Two studies indicated an adequate progesterone opposing effect by the same lead author (1: Only 28 days duration; dose of progesterone cream was at 15 mg bid or 40 mg bid) (2: 6 months duration; 40 mg cream continuous). The 6-month study of 40 mg cream per day did have 19% of the women showing proliferative endometrium, but no hyperplasia on biopsy. The remaining 3 studies did not have an adequate progesterone cream opposing effect, showing proliferative endometrium and two cases of complex hyperplasia, and no endometrial cancer. One of the negative studies, the one with complex hyperplasia, was 48 weeks duration; two of the negative studies were 12 weeks duration.
In general, these studies were too short and too few, and showed concerning cases of endometrial thickening, hyperplasia, and complex hyperplasia, even in these short durations. Endometrium being stimulated by systemic estrogen with unopposed progestogens in women with a uterus tend to get thicker, more proliferative, and more hyperplastic with increased risk of atypia and cancer over time.
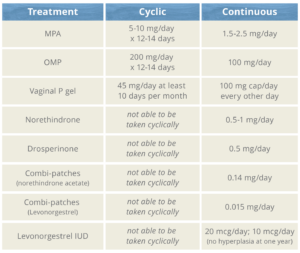
Here are the doses that are used to provide adequate endometrial protection when systemic estrogen is given in average or lower than average doses. If twice the average dose of estrogen is used (maximum would be oral estradiol 2 mg/day or patch estradiol 0.1 mg/day) it is unclear if one should use the doses below or increase the doses below. For oral micronized progesterone, I highly recommend 200 mg OMP for any dose of estrogen above average (oral 1 mg estradiol, or patch 0.05 mg).
Become a DUTCH Provider to learn more about how hormone testing can help inform comprehensive patient treatment plans.
References
Leonetti H, Wilson K, Anasti J. Topical progesterone cream has an antiproliferative effect on estrogen-stimulated endometrium. Fertil Steril 2003; 79:221-222.
Leonetti H, Steinberg J, Anasti D, James, N. TRANSDERMAL PROGESTERONE CREAM AS AN ALTERNATIVE PROGESTIN IN HORMONE THERAPY. Alternative Therapies in Health and Medicine; Aliso Viejo Vol. 11, Iss. 6, (Nov/Dec 2005): 36-8.
Vashisht A, Wadsworth F, Carey A, et al. Bleeding profiles and effects on the endometrium for women using a novel combination of transdermal oestradiol and natural progesterone cream as part of a continuous combined hormone replacement regime. BJOG 2005;112:1402-1406.
Wren B, McFarland K, Edwards L. Micronised transdermal progesterone and endometrial response. Lancet 1999; 354:1447-8
Jane F, Davis S. A practitioner’s toolkit for managing the menopause. Climacteric 2014;17:564-79.
Mueck A, Romer T. Choice of progestogen for endometrial protection in combination with transdermal estradiol in menopausal women. Hormone Molecular Biology and Clinical Investigation 2019: 201
Lie J. What providers need to know about progestogens in hormone therapy. NAMS Practice Pear 2020; Sept 10.
Stute P, Neulen J, Wildt. The im6-328pact of micronized progesterone on the endometrium: a systematic review. Climacteric 2016; 19(4): 31
This post was written by our guest author, Dr. Tori Hudson, ND.
Dr. Hudson is clinical adjunct professor at NUNM, Southwest College of Naturopathic Medicine, Bastyr University and the Canadian College of Naturopathic Medicine. Dr Hudson has been in practice for more than 36 years, is the medical director of “A Woman’s Time” in Portland, Oregon, co-owner and director of product research and education for VITANICA, and the program director for the Institute of Women’s Health and Integrative Medicine. She is also the founder and co-director of NERC (Naturopathic Education and Research Consortium), a non-profit organization for accredited naturopathic residencies. Dr. Hudson has been appointed as a faculty member of the Fellowship in Integrative Health and Medicine, Academy of Integrative Health & Medicine.
Learn More about Dr. Tori Hudson
TAGS
Women's Health
Hormone Replacement Therapy (HRT)
Endometrial Health
Postmenopausal Women
Menopause
Estrogen and Progesterone