Get your ticket to DUTCH Fest 2026! Join us March 12-14 in Dallas, TX for cutting-edge hormone education and hands-on learning. Learn more and register today.*
*DUTCH Fest is exclusive to registered DUTCH Providers. Only registered DUTCH Providers can attend.
Improving Treatment Plans for PCOS and Pregnancy
Kelly Ruef, ND
Improving Treatment Plans for PCOS and Pregnancy
by Kelly Ruef, ND
PCOS is a common hormonal disorder among women of reproductive age. PCOS affects an astounding number of women in the US (between six and 12 percent). Because it often results in infrequent or absent ovulation, PCOS can pose a challenge to those who are trying to conceive.
The good news is that PCOS-related infertility can be successfully treated in many women by both conventional and functional medicine approaches. These approaches can be more personalized and effective with the help of comprehensive hormone testing.
Diagnosing PCOS
PCOS is a diagnosis of exclusion, meaning that providers must first rule out other common conditions that can present with similar symptoms, such as:
- hypothyroidism
- hyperprolactinemia
- nonclassical congenital adrenal hyperplasia (NCAH)
- Cushing’s syndrome
- hypogonadotropic hypogonadism
- primary ovarian insufficiency (POI)
- androgen-secreting tumors.
A ccording to the 2003 Rotterdam Criteria, PCOS is defined by the presence of at least two of three of following: oligo-anovulation, hyperandrogenism (elevated androgens), and/or polycystic ovaries on ultrasound.
On lab work for patients with PCOS, providers often see imbalances in:
- Hormones (elevated androgens like DHEAS and testosterone and low SHBG)
- Blood sugar (elevated fasting glucose, HbA1c, fasting insulin, etc.)
- Brain-ovarian signaling (increased LH/FSH ratio)
- Inflammation (elevated CRP-hs and SED rate)
- Fats (dyslipidemia – low HDL and elevated LDL and triglycerides)
- Ovarian function (polycystic ovarian morphology (PCOM) on ultrasound, elevated AMH)
These imbalances can increase the risk for developing type 2 diabetes, cardiovascular disease, endometrial and breast cancers, and infertility. Thus (besides improving symptoms, regulating cycles, and improving fertility) PCOS treatment goals should also focus on minimizing these risks.
PCOS and Pregnancy
So why do women with PCOS have trouble becoming pregnant? One obvious answer is that many women with PCOS go months (or longer) without ovulating. Reasons for anovulation are likely multifactorial and different for every woman, but one contributing factor is high androgens.

Androgens tend to elevate in response to insulin resistance, inflammation, stress and dysregulated brain-ovarian signaling—all present in cases of PCOS. Once elevated, these androgens prevent a dominant follicle from being selected in the follicular phase. Instead of one, large, mature follicle in the ovary, we see many, small, immature follicles that are not ready to or able to ovulate an egg.
Improving the body’s ability to mature a dominant follicle in a timely manner may improve pregnancy rates in women with PCOS. The degree of medical intervention that is needed to accomplish this will be different for every woman.
PCOS is a syndrome with many possible causes and clinical presentations—some women with PCOS may get pregnant naturally with minimal or no medical intervention while other women may require fertility medications (clomid, letrozole, etc.).
Treatment Options for PCOS
Conventional treatments for PCOS often include metformin to regulate blood sugar, spironolactone to decrease androgens and related symptoms, and/or birth control pills (or cyclic progestin therapy, mini-pill or progestin IUD) to reduce the risk of endometrial hyperplasia.
Please note that when a woman with PCOS is trying to conceive, she must work with her physician to stop the spironolactone and the birth control.
Alternative treatments for PCOS include turmeric, n-acetylcysteine (NAC), white peony, licorice, zinc, myoinositol, green tea, EGCG, gymnema, chromium, saw palmetto, nettle root, pygeum, reishi mushrooms, vitex, fish oil, resveratrol, berberine, cinnamon, B-vitamins, vitamin C, vitamin D, fenugreek, L-carnitine, CoQ10, spearmint tea, chamomile, maitake mushrooms, black cohosh and flaxseeds.
Comprehensive Hormone Testing Can Help Personalize PCOS Treatment Plans
With so many available treatment options, it’s difficult to know which route to take. This is where comprehensive hormone testing can make the difference between a routine therapy and a personalized treatment plan. Precision Analytical offers various hormone testing panels that can help a provider know, for example, if saw palmetto or that white peony/licorice blend will be most helpful to the patient.
Androgens and Their Metabolites
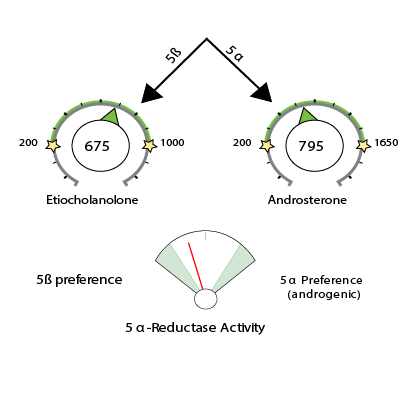
The DUTCH Complete and DUTCH Plus tests provide a comprehensive picture of androgen levels. Providers can see DHEAS and testosterone levels, and learn how these two androgens are being metabolized by looking at the ratios of their five downstream alpha and beta metabolites.
In PCOS, providers will often see elevated androgens and a metabolism preference for the more androgenic, alpha pathway. When a woman prefers the alpha pathway, she tends to push her androgens into more potent forms like 5a-DHT which can lead to symptoms of elevated androgens. If a woman heavily prefers the alpha pathway, we might work to regulate insulin, but we may also utilize 5a-reductase blockers such as saw palmetto, nettle root, EGCG, pygeum, reishi mushrooms and zinc.
Estrogens and Their Metabolites
The DUTCH Test also measures estrogens (E1, E2 and E3) and their downstream metabolites. We know that in some women with PCOS, aromatase (CYP19A1) is genetically downregulated, resulting in less androgen-to-estrogen conversion. If E1, E2 and E3 levels come back low on the DUTCH Test, providers might consider agents that push aromatase activity, like white peony/licorice blend. And providers might consider phytoestrogens via black cohosh and flaxseeds.
Conversely, if estrogen levels come back elevated on the DUTCH Test, providers might use agents to improve the patient’s metabolism and clearance, such as DIM, rosemary, resveratrol, cruciferous vegetables, sulforaphane, B vitamins, magnesium, etc.
Adrenal Hormones
The DUTCH Test may also help a provider understand if the adrenals are contributing to the high androgen picture. Many times, the elevated androgens seen in PCOS are due to overproduction by the ovaries in response to insulin resistance and dysregulated brain-ovarian signaling. However, the adrenals can also overproduce androgens.
If a woman has high free cortisol and cortisone and high metabolized cortisol on her DUTCH Test, then it might be more likely that her adrenals are contributing to the high androgens. With high cortisol, a provider might consider adrenal support with stress reduction, B vitamins, vitamin C, and calming adaptogens such as holy basil.
Estrogen/Progesterone Balance
Providers can also see the balance between estrogen and progesterone on the DUTCH Test. Many times, providers will see a low progesterone to estrogen ratio in women with PCOS. This can be attributed to the fact that it is common for women with PCOS to ovulate very infrequently or not at all, and as a result go long periods of time without exposure to progesterone.
This reduced exposure to progesterone overtime can increase risk for endometrial hyperplasia and cancer and breast cancer. If a woman with PCOS is struggling to ovulate, or if her progesterone levels are low, her provider might consider stress reduction, regulating blood sugars with myoinositol, fenugreek and/or chromium, lowering inflammation with NAC, resveratrol, EGCG and/or borage oil, or modulate LH signaling with vitex for her treatment plan.
Personalized Treatment Plans Can Help Women with PCOS
These are just a few examples of how the DUTCH Test can aid in creating more personalized treatment plans for women with PCOS who want to become pregnant. Keep in mind that some supplements and medications need to be discontinued once a successful pregnancy has occurred.
With the help of comprehensive hormone testing, women with PCOS-related infertility can gain access to better, more personalized treatment protocols that can increase their chances of becoming pregnant and improve their long-term health. You can learn more about diagnosing and treating PCOS in my recent case study on the DUTCH website.
Kalra B, Kalra S, Sharma JB. The inositols and polycystic ovary syndrome. Indian J Endocrinol Metab. 2016 Sep-Oct;20(5):720-724. doi: 10.4103/2230-8210.189231. PMID: 27730087; PMCID: PMC5040057.
Kamel HH. Role of phyto-oestrogens in ovulation induction in women with polycystic ovarian syndrome. Eur J Obstet Gynecol Reprod Biol. 2013 May;168(1):60-3. doi: 10.1016/j.ejogrb.2012.12.025. Epub 2013 Jan 21. PMID: 23347605.
Panghiyangani R, Soeharso P, Andrijono, Suryandari DA, Wiweko B, Kurniati M, Pujianto DA. CYP19A1 Gene Expression in Patients with Polycystic Ovarian Syndrome. J Hum Reprod Sci. 2020 Apr-Jun;13(2):100-103. doi: 10.4103/jhrs.JHRS_142_18. Epub 2020 Jul 9. PMID: 32792756; PMCID: PMC7394102.
Pasquali R. Contemporary approaches to the management of polycystic ovary syndrome. Ther Adv Endocrinol Metab. 2018 Apr;9(4):123-134. doi: 10.1177/2042018818756790. Epub 2018 Feb 7. PMID: 29619209; PMCID: PMC5871061.
“PCOS (Polycystic Ovary Syndrome) and Diabetes.” Centers for Disease Control and Prevention , CDC, 24 Mar. 2020, https://www.cdc.gov/diabetes/basics/pcos.html.
Takahashi K, Kitao M. Effect of TJ-68 (shakuyaku-kanzo-to) on polycystic ovarian disease. Int J Fertil Menopausal Stud. 1994 Mar-Apr;39(2):69-76. PMID: 8012442.
TAGS
Women's Health
Pregnancy/Postpartum
Premenopausal Women
Polycystic Ovary Syndrome (PCOS)
Medications and Supplements
HPA Axis
Estrogen and Progesterone
Androgens (Testosterone/DHEA)
Adrenal Androgens (DHEA)
Obesity
Insulin Resistance
Hair Loss
Inflammation