Get your ticket to DUTCH Fest 2026! Join us March 12-14 in Dallas, TX for cutting-edge hormone education and hands-on learning. Learn more and register today.* Early bird pricing ends January 31!
*DUTCH Fest is exclusive to registered DUTCH Providers. Only registered DUTCH Providers can attend.
The Relationship Between HPA Axis Function and BMI
Jaclyn Smeaton
The Relationship Between HPA Axis Function and BMI
by Jaclyn Smeaton, ND
Obesity in America has reached pandemic levels, and with the increased prevalence, there has been an increasing focus on the underlying drivers of obesity. The main focus used to be on simply a mathematical equation: calories in, calories out. Yet, this model has failed to explain many cases of obesity.
A Broader Approach to Understanding BMI
Research insights have helped to expand the pathophysiological understanding of obesity with help from a broader focus on researching conditions such as type 2 diabetes, hypertension, dyslipidemia, and hypothalamic-pituitary-adrenal (HPA) axis disorders. This has resulted in a broader approach to body mass index (BMI) and weight management through increased insulin sensitivity, appetite suppression, and more recently, HPA axis management.
The integrative medicine community has been aware of this connection for some time through clinical observation, but there has not been much research to date exploring this in more detail.

However, if we look at diseases of the HPA axis, notably Cushing’s disease and Addison’s disease, we can observe effects on BMI. Cushing’s disease, characterized by cortisol excess, is associated with increased BMI. Similarly, the administration of glucocorticoids as medications are also known to lead to weight gain . Alternately, Addison’s disease, which is characterized by hypocortisolism, is associated with weight loss (or a decrease in BMI).
While we have examples of disease states of over and underproduction of cortisol impacting weight and BMI, there hasn’t been as much research completed to date looking at a more mild or moderate state of HPA axis dysregulation, like what we see more commonly among our patient populations. The data that exists which evaluates the association between cortisol and BMI is often contradictory and uses different measures of cortisol (morning, diurnal pattern, CAR) and measurement in different fluids (saliva, serum, urine). Most studies, with very few exceptions, have also been very small. Studies evaluating the relationship between cortisol metabolites and BMI have shown a more consistent association.
DUTCH Research on Moderate HPA Axis Dysregulation
In October 2023, the research team at DUTCH published the first comprehensive study of this kind, using both saliva and dried urine measurements and looking at a more diverse assessment of HPA axis function including cortisol, cortisone, and cortisol metabolites. This study included patients aged 19-85 years with a BMI between 16 and 60 kg/m 2 . It excluded individuals who were pregnant, taking hormonal medication, or reporting adrenal or thyroid disease. It also excluded those who woke to urinate at night, as that can temporarily inhibit cortisol secretion, and those with renal disease or overly dilute urine. In all, the study included 23,988 individuals who had completed the DUTCH Complete (urine only) and 4,892 who had completed the DUTCH Plus (urine and saliva).
DUTCH Research Findings
This study showed a clinically significant correlation (defined as a correlation coefficient larger than 0.1) between cortisolmetabolites and BMI, but not salivary or urinary free cortisol. A few additional key findings included:
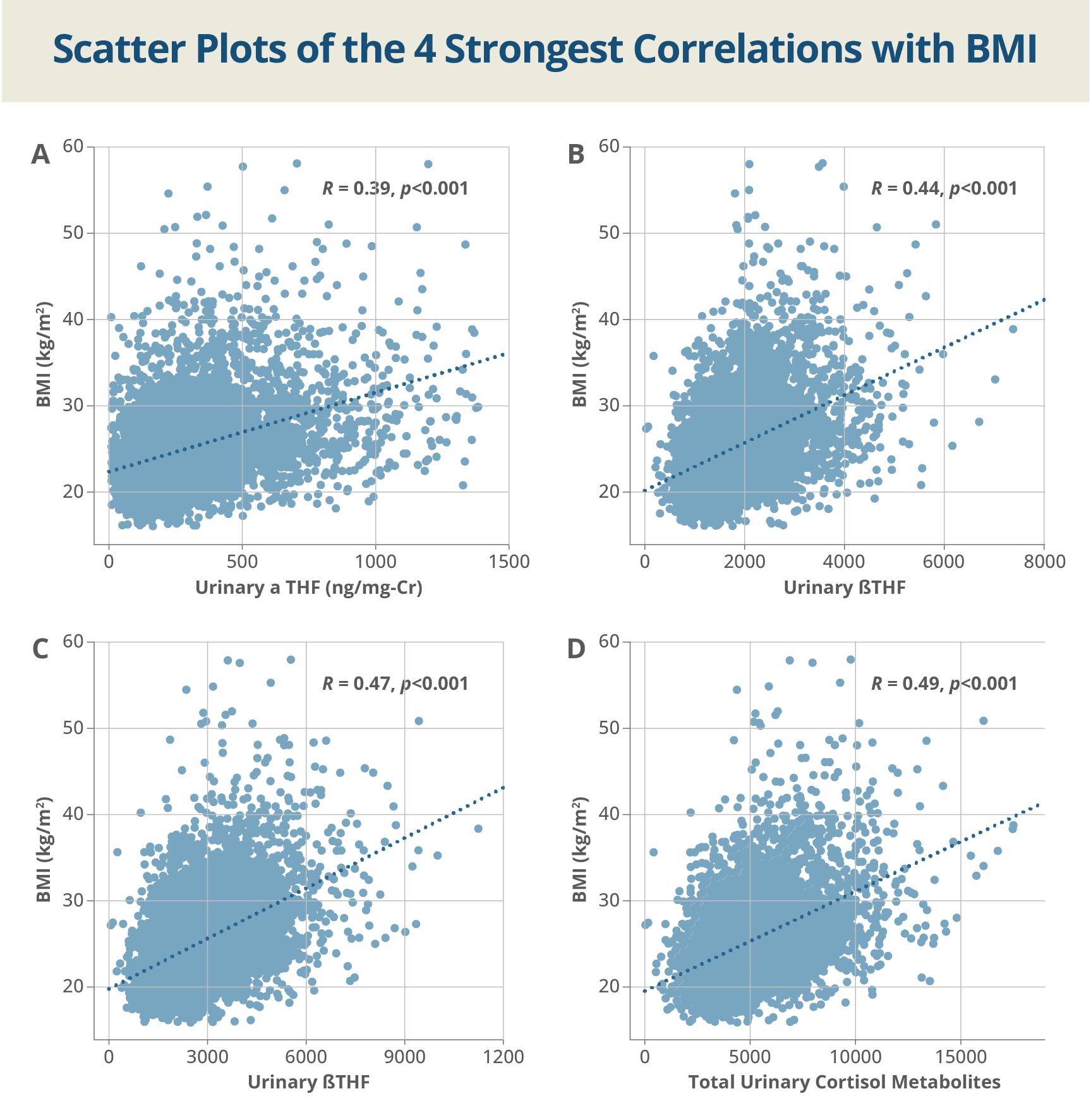
- Cortisol metabolites, including aTHF, bTHF, and total cortisol metabolites (TCM) all had moderate, positive correlations with BMI, meaning that they were higher in individuals with a higher BMI.
- In the 16.2% of individuals categorized as obese (BMI > 30 kg/m 2 ), a relatively larger percentage (32%) had a THE concentration higher than the upper reference range compared to only 8.3% of those who were not obese.
- This trend held for aTHF and bTHF as well.
- The odds of an individual with an obese BMI having an elevated THE were 7.43 times that of a person with a nonobese BMI.
- The odds of an individual with an obese BMI having an elevated aTHF and bTHF were 6.2 times that of a person with a nonobese BMI.
- There were 638 individuals who returned for repeat lab testing at least 90 days after their initial evaluation. In these patients, baseline THE was associated with a change in BMI after accounting for initial BMI, and initial total cortisol metabolites (TCM) were also associated with changes in BMI.
- After controlling for age, sex, menstrual status, and concentrations of testosterone, b-pregnanediol, and urinary creatinine, 29% of the variability in BMI can be explained by urinary cortisol metabolites, suggesting this plays a significant role in weight regulation
If you’re interested in reading the details of the paper and the regression analyses, check out the full paper .
Theories on the HPA Axis and BMI Connection
There has been a bit of exploration about why there would exist an association between cortisol metabolites and BMI and several theories have been postulated. The most commonly discussed theory suggests there is an increase in peripheral metabolism and clearance of cortisol in obese individuals. Another leading theory is that there is a change in central HPA axis control in obese individuals. Our data suggests that both might be happening.
Various factors can stimulate the HPA axis to increase cortisol production, including stress, inflammation, and more. When this occurs, cortisol clearance is increased in order to compensate and keep a stable concentration of free cortisol. This increased peripheral metabolism is thought to be caused by an increase in 5a-reductase activity as well as a decrease in conversion of cortisone to cortisol in the liver. This would, in theory, lead to increasing levels of the cortisone metabolite, THE. In addition, in obesity, adipose tissue sequesters cortisol which in turn might further increase cortisol production.
Increased Cortisol Clearance Rate in Your Patients
You may have seen examples of this in your own patient population, where you might observe an increased cortisol clearance rate (CCR). In the DUTCH Interpretive Guide , this is discussed in detail on page 116. Cortisol clearance rate can be observed through comparison of the 24-hour free cortisol (4 timepoints of measurement in saliva or urine) to the metabolized cortisol (THF + THE). If the metabolized cortisol is relatively higher than free cortisol, this suggests an increased cortisol clearance rate. The guide explains how CCR can be associated with obesity, inflammation, blood sugar and insulin dysregulation, and long-term stress.
There has been an attempt to target the HPA axis as a means to treat obesity and metabolic syndrome, notably through development of 11 beta-hydroxysteroid dehydrogenase (11b-HSD) type 1 inhibitors ( Freude , Anagnostis ). Investigators involved in that work have described that 11b-HSD activity “seems to be dependent on BMI”, and research in mice models has suggested that overexpression of 11b-HSD1 (which converts cortisone to cortisol) is associated with obesity. Although there are conflicting results, that same phenomenon is thought to apply to humans as well.
HPA Axis Function and Weight Management
When it comes to weight management, HPA axis function appears to be a very important factor to consider. Our data suggests that HPA axis evaluation may be a valuable tool to gain insights into causes for idiopathic obesity. Results might suggest that there could be additional lifestyle factors that are causing weight gain which could trigger additional evaluation or discussion. These could include several causes of HPA axis dysfunction including poor sleep habits, chronic inflammation, increased sugar consumption, and an increase in emotional stress.
The good news is that this can be managed in patients with an increased BMI or those struggling with weight management. Practitioners may work to reduce chronic inflammation through the use of therapeutic diet protocols like the anti-inflammatory or Mediterranean diets. Where blood sugar dysregulation or insulin resistance is suspected, nutritional approaches may be executed, and even paired with supplements like Gymnema, chromium, berberine and others. Finally sleep and stress may be addressed through lifestyle management, a focus on circadian health, stress management and support for the parasympathetic nervous system, and by providing calming botanicals, adrenal adaptogens, or GABA support.

Whatever therapeutic approach seems best for your patient, consideration of HPA axis function and, in particular, cortisol metabolism, appears to be a very important factor to address in patients trying to manage their weight.
TAGS
Perimenopause
Weight Management
Obesity
General Health
HPA Axis
Cortisol
Insulin Resistance
Polycystic Ovary Syndrome (PCOS)