DUTCH Fest 2026 is sold out! Join the list to get notified about our next DUTCH Fest.
The Role of Hormones in Men's Health
Cameron Craw, ND
As men age, the risk of various health concerns ranging from cardiovascular disease, metabolic dysfunction, changes in body composition, reduced exercise stamina, and many others, increase. With many men’s health issues so closely tied to hormonal imbalance, a clinical evaluation often starts by assessing hormone levels through comprehensive men’s hormone tests. These tests help clinicians understand how well the body’s systems are working together. While testosterone is the central male hormone, it is only part of the picture. Other hormones—like dihydrotestosterone (DHT), prolactin, and estrogens to name a few—also play important roles in shaping men’s hormonal health and mental health. Taking a broader look at all these hormones helps guide more personalized approaches to restoring vitality.
Low Testosterone
Many men face challenges related to low testosterone, which can have a far-reaching impact on daily life and overall wellbeing. Low testosterone, also known as hypogonadism, can lead to persistent fatigue, reduced strength and muscle mass, increased body fat, and a noticeably lower sex drive or difficulties with sexual function. Other effects may include mood changes like depression or irritability, difficulty concentrating, poor sleep, and even changes in hair growth or bone health.
Over recent decades, the prevalence of low testosterone has steadily increased among men in many age groups, with some studies projecting that as many as 6.5 million American men ages 30 to 79 will have symptomatic testosterone deficiency by 2025—a nearly 40% rise since 2000.1 Factors thought to contribute to this trend include an aging population, higher rates of obesity and chronic illness, and possible environmental or lifestyle changes.1
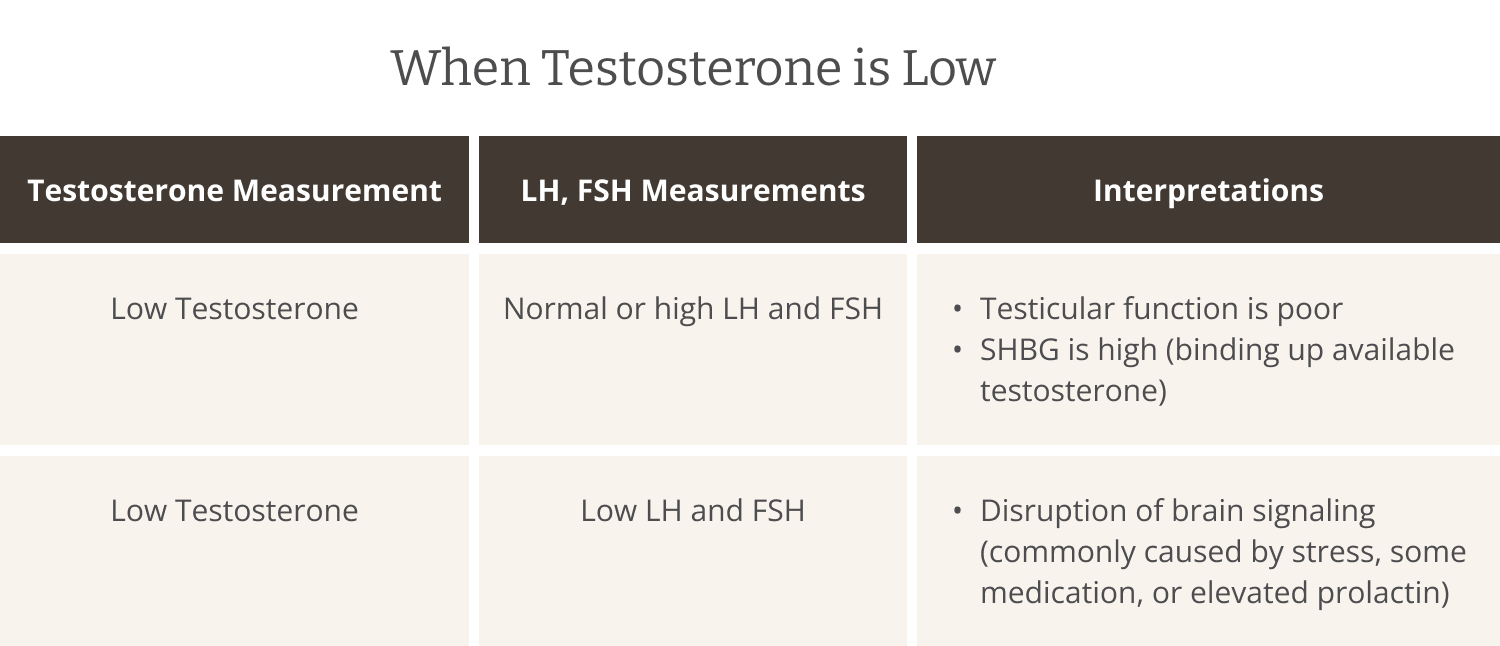
In men's health, a key hormone pathway can be found between the brain and the testicles (testes). Even with the vast majority of testosterone produced by the testes, low testosterone can result from problems within the brain as well as the testes. By measuring not only testosterone but also luteinizing hormone (LH) and follicle-stimulating hormone (FSH), clinicians can determine whether the issue is primary, meaning the testes are failing despite strong signals from the brain, or secondary, meaning the brain itself is sending weak or inadequate instructions.
Additionally, prolactin, a hormone produced by the brain, can strongly influence testosterone levels by disrupting the communication between the brain and the testes. High prolactin levels suppress the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the brain’s pituitary gland. When this signaling pathway is blocked, testosterone production decreases even if the testes themselves are healthy and the pituitary gland is otherwise functional. Proper brain-to-testes communication is vital for maintaining normal testosterone levels and overall male reproductive health.
Other hormone measurements—like estradiol, sex hormone-binding globulin (SHBG), and Dehydroepiandrosterone sulfate (DHEAS)—can also help explain why testosterone may be low or otherwise ineffective. Too much estradiol (a form of estrogen) can interfere with testosterone by disrupting its normal actions and reducing its levels through feedback mechanisms in the brain. High or low SHBG affects how much testosterone is bound up in the blood, which can affect how much active testosterone is available for use by the body’s cells. DHEAS, a hormone made by the adrenal glands, supports hormone balance because the body can convert it into testosterone or estrogen as needed. By looking at all these markers together, doctors can better understand whether low testosterone is caused by problems in the testes, the brain, or elsewhere.
High Testosterone
Many men's health issues are negatively impacted by high testosterone levels or by excessive activity of testosterone metabolites such as dihydrotestosterone (DHT). DHT functions as a super potent form of testosterone. In individuals with genetic susceptibility, elevated DHT levels often contribute to or worsen various men's health conditions. Male pattern baldness affects approximately 50% of men by the age of 50, and DHT is a central factor in its development.2 Prostate enlargement is another common condition linked to high local DHT activity, affecting a majority of men over 60 to varying degrees and often causing urinary symptoms.3 While circulating DHT levels alone have not been definitively linked to prostate cancer risk, the enzyme activity converting testosterone to DHT in prostate tissue is critical for disease progression in genetically predisposed men.4
These conditions underscore the importance of understanding not only the primary hormones, like testosterone, but also their downstream metabolites, like DHT, when conducting a comprehensive clinical evaluation. Given that the effects of hormone metabolites can differ significantly from those of their parent hormones, a common way to impact the prevalence and activity of different hormones is through modifying the activity of enzymes that create them. For instance, the enzyme 5 alpha-reductase converts testosterone into the more potent dihydrotestosterone (DHT), allowing local regulation of hormone levels in tissues such as the prostate, skin, and hair follicles. Due to its pivotal role, 5 alpha-reductase is a key therapeutic target; inhibitors of this enzyme are used to lower DHT levels (measured by way of the urinary DHT metabolite 5a-androstenediol) and manage conditions like prostate enlargement and male pattern balding.
Hormone Therapy for Men
Hormone therapy involves the introduction of hormone(s) into the body from an external source, usually aimed at restoring hormonal balance. In men diagnosed with hypogonadism, testosterone therapy is often used. This can improve a variety of issues including low libido, decreased muscle mass, fatigue, mood disturbances, and low bone density. While testosterone therapy offers these potential benefits, it is important to recognize that it is not without risks. Some men may experience adverse effects such as worsening sleep apnea, elevated red blood cell counts, acne, and breast tenderness. Moreover, because testosterone can be converted into DHT, hormone therapy must be carefully managed to avoid exacerbating conditions like prostate disease or male pattern baldness. Appropriate patient selection, thorough men’s hormone tests to confirm deficiency, and ongoing monitoring by healthcare professionals are essential to maximize benefits and minimize risks during treatment.
In younger men, testosterone replacement is applied with heightened caution due to its potential for prolonged LH and FSH suppression after testosterone discontinuation. This suppression can reduce or even halt intrinsic testosterone and sperm production, sometimes leading to persistent hypogonadism for more than a year after therapy ends.5 For this reason, clinicians often explore strategies to preserve fertility and natural endocrine function before considering testosterone replacement. One such strategy incorporates a hormone called human chorionic gonadotropin (hCG) to stimulate LH activity, thereby maintaining testicular function. hCG therapy helps preserve the natural testosterone regulatory feedback loop between the brain and testes, supporting ongoing testicular function even during treatment.
Beyond Testosterone Therapy
Dietary choices rich in zinc, vitamin D, and healthy fats can support natural testosterone production and overall hormone health, which may also aid weight loss efforts.6 Regular exercise, particularly strength training, helps maintain muscle mass and boosts testosterone levels, at least in the short term.7 Stress reduction techniques and sufficient sleep are also critical since stress hormones like cortisol can suppress testosterone production.8 Herbs such as ashwagandha, fenugreek, and Asian reg ginseng show promise in supporting healthy testosterone levels.9 Additionally, natural compounds that inhibit enzymes like aromatase or 5-alpha-reductase can help modify hormone metabolism and reduce the effects of excessive testosterone metabolites. While these approaches may not fully replace hormone therapy for those with significant deficiencies, many men benefit from integrating lifestyle modifications and supplements to improve symptoms, quality of life, and potentially delay or reduce the need for pharmacological intervention.
Conclusion
Men's health is linked to a complex and dynamic hormonal environment shaped by genetics, anatomy, and endocrine function. Understanding the full spectrum of male hormones—including testosterone, its metabolites, and other regulators like prolactin and estradiol—is essential for diagnosing and managing common conditions such as low testosterone, male pattern baldness, and prostate health issues. Comprehensive hormone testing facilitates a more personalized treatment approach that can address the root causes of many imbalances, whether originating in the brain, testes, or peripheral metabolism. While hormone therapy remains a cornerstone for treating true deficiencies, lifestyle factors including nutrition, herbal medicine, exercise, sleep, and stress management are all valuable tools for addressing hormonal balance naturally. This holistic approach can empower men to better maintain vitality and quality of life by nurturing their masculinity from within.
References
[1] Kahl KL. Testosterone levels show steady decrease among young US men. Urology Times. . Published January 26, 2022. Accessed October 12, 2025.
[2] Ellis JA, Stebbing M, Harrap SB. Androgenetic alopecia: pathogenesis and potential for therapy. Expert Rev Mol Med. 2002;4(22):1-11. doi:10.1017/S1462399402005433.
[3] Tong Y, Zhou RY. Review of the Roles and Interaction of Androgen and Inflammation in Benign Prostatic Hyperplasia. Mediators Inflamm. 2020;2020:7958316. Published 2020 Oct 28. doi:10.1155/2020/7958316
[4] Lundgren PO, Kjellman A, Norming U, Gustafsson O. Association between dihydrotestosterone and long-term risk for prostate cancer mortality: A prospective cohort study. Prostate. 2020;80(10):777-781. doi:10.1002/pros.23991
[5] Handelsman DJ, Desai R, Conway AJ, et al. Recovery of male reproductive endocrine function after ceasing prolonged testosterone undecanoate injections. Eur J Endocrinol. 2022;186(3):307-318. Published 2022 Jan 28. doi:10.1530/EJE-21-0608
[6] Zamir A, Ben-Zeev T, Hoffman JR. Manipulation of Dietary Intake on Changes in Circulating Testosterone Concentrations. Nutrients. 2021;13(10):3375. Published 2021 Sep 25. doi:10.3390/nu13103375
[7] D'Andrea S, Spaggiari G, Barbonetti A, Santi D. Endogenous transient doping: physical exercise acutely increases testosterone levels-results from a meta-analysis. J Endocrinol Invest. 2020;43(10):1349-1371. doi:10.1007/s40618-020-01251-3
[8] Harden KP, Wrzus C, Luong G, et al. Diurnal coupling between testosterone and cortisol from adolescence to older adulthood. Psychoneuroendocrinology. 2016;73:79-90. doi:10.1016/j.psyneuen.2016.07.216
[9] Smith SJ, Lopresti AL, Teo SYM, Fairchild TJ. Examining the Effects of Herbs on Testosterone Concentrations in Men: A Systematic Review. Adv Nutr. 2021;12(3):744-765. doi:10.1093/advances/nmaa134
TAGS
Men's Health
Testosterone
Estrogen
Hormone Replacement Therapy (HRT)
General Hormone Health