Menopause for Men: What Does Low Estrogen Mean?
by Tim Hyatt, ND
If you are a male, you have likely heard or read about declining testosterone (low T). Testosterone production does decrease with age, but it can also decrease faster from poor lifestyle choices, chemicals in the environment, and conditions such as obesity and diabetes. This creates a host of symptoms such as low sex drive, poor sexual function, decreased muscle mass or the inability to increase it, anxiety, slow healing, low motivation, and more.
While declining testosterone in men is definitely a problem, we also know estrogen can be just as important when it comes to hormone balance as a man ages. Researchers have discovered that just as women go through menopause due to a dramatic decrease in estrogen product, middle-aged men also undergo estrogen-related changes in body composition and sexual function.
A study published in The New England Journal of Medicine was conducted by researchers at Massachusetts General Hospital (MGH) which found that a diagnosis of male hypogonadism (a drop in reproductive hormone levels high enough to cause physical symptoms) is traditionally made based on blood testosterone levels. However, there is little understanding of the levels of testosterone needed to support certain functions.
According to the study authors, a small proportion of the testosterone made by men is usually converted into estrogen by aromatase, a type of enzyme, and the higher the testosterone level in a man, the more testosterone is converted into estrogen.
If the aromatase enzyme is upregulated, a man will become estrogen dominant. The major clinical signs of estrogen excess in men are gynecomastia (breast development), testicular atrophy, erectile dysfunction, depression, and infertility. Another potential effect includes a significantly increased risk for type-2 diabetes. We know excess estrogen also causes water retention (less frequent urination) in both men and women, which can lead to excessive sweating, blood pressure spikes or high blood pressure, insomnia, hot flushing around the ears or on the face, night sweats, and brain fog.
On the flip side, what if men do not have enough estrogen? Estrogen is required for the activation of testosterone receptors and, in the presence of very low estrogen this triggers, a loss of testosterone receptors. This decline in the number of testosterone receptors can have a dramatic impact the body because testosterone will not have anywhere to bind and create action. In the same study referenced above, authors developed a testing method using various combinations of testosterone, estrogen, anastrozole, and goserelin acetate and found that “estrogen deficiency primarily accounted for increases in body fat, and both contributed to the decline in sexual function.” This data confirms that testosterone is not the only important player when it comes to men’s sexual and overall health.
Another study shows cortical bone is depleted when estrogen levels are low. This puts men at risk for osteoporosis. Once again, it is the balance of testosterone and estrogen that is important! For a long time medical professionals have thought estrogen is detrimental to a man's well-being, but we now know that is not entirely true.
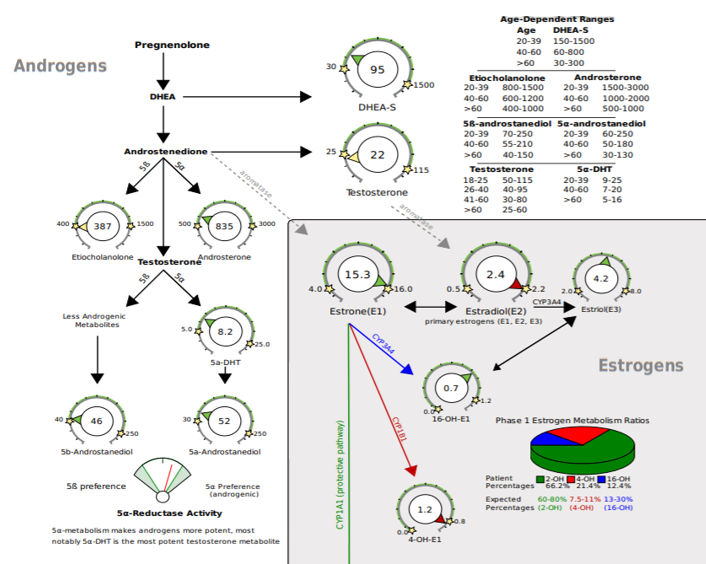
Men should test their hormone levels to detect and correct imbalances associated with symptoms. Testosterone and its metabolites and estrogen metabolism are all reported on the male sex hormone pages of the DUTCH Test®. This allows practitioners to fully evaluate the androgens such as DHEA-S, testosterone, 5a-DHT, 5a and 5b-androstanediol, etiocholanolone, and androsterone. In addition, the three main estrogens (estrone, estradiol, and estriol) plus estrogen metabolism will show if a male patient is estrogen dominant or estrogen deficient and how his estrogen detoxification is working. Better patient outcomes can be achieved when evaluating these two hormone sections in tandem.
References
Estrogen and the Male, Judy K. Lee, Julianne Imperato-McGinley, in Encyclopedia of Endocrine Diseases, 2004.
Diabetes Care. 2013 Sep; 36(9): 2591–2596. Published online 2013 Aug 13. doi: 2337/dc12-2477.
Circulating Estrone Levels Are Associated Prospectively With Diabetes Risk in Men of the Framingham Heart Study, Guneet Kaur Jasuja, PHD,1,2 Thomas G. Travison, PHD,3,4 Maithili Davda, MPH,3 Adam J. Rose, MD,2,5 Anqi Zhang, PHD,3 Mark M. Kushnir, PHD,6 Alan L. Rockwood, PHD,6 Wayne Meikle, MD,6 Andrea D. Coviello, MD, MS,3,7 Ralph D’Agostino, PHD,1,2 Ramachandran S. Vasan, MD,7,8 and Shalender Bhasin, MD3
Gonadal Steroids and Body Composition, Strength, and Sexual Function in Men, Joel S. Finkelstein, M.D., Hang Lee, Ph.D., Sherri-Ann M. Burnett-Bowie, M.D., M.P.H., J. Carl Pallais, M.D., M.P.H., Elaine W. Yu, M.D., Lawrence F. Borges, M.D., Brent F. Jones, M.D., Christopher V. Barry, M.P.H., Kendra E. Wulczyn, B.A., Bijoy J. Thomas, M.D., and Benjamin Z. Leder, M.D., N Engl J Med 2013; 369:1011-1022 September 12, 2013DOI: 10.1056/NEJMoa1206168.
Serum estradiol levels are inversely associated with cortical porosity in older men. Vandenput L1, Lorentzon M, Sundh D, Nilsson ME, Karlsson MK, Mellström D, Ohlsson C.,J Clin Endocrinol Metab. 2014 Jul;99(7):E1322-6. doi: 10.1210/jc.2014-1319. Epub 2014 Apr 2.
The effect of estrogen and androgen on androgen receptors and mRNA levels in uterine leiomyoma, myometrium and endometrium of human subjects. Fujimoto J1, Nishigaki M, Hori M, Ichigo S, Itoh T, Tamaya T., J Steroid Biochem Mol Biol. 1994 Aug;50(3-4):137-43.
The role of estradiol in male reproductive function, Michael Schulster,1 Aaron M Bernie,1 and Ranjith Ramasamy 2 J Clin Endocrinol Metab. 2014 Jul;99(7):E1322-6 doi: 10.1210/jc.2014-1319. Epub 2014 Apr 2.