Metabolized Versus Free Cortisol: Understanding the Difference
by Carrie Jones, ND, MPH
The DUTCH Test™ is well-recognized for its reporting that is not available from other laboratories. The cortisol metabolites in the adrenal section are among the commonly highlighted markers appreciated by practitioners. They offer a much more complete view of the HPA axis when taken into consideration with the free cortisol.
Cortisol is made from cholesterol in the zona fasciculata layer of the adrenal cortex. Eighty to 90% of cortisol is bound to cortisol-binding globulin (CBG), much like thyroid hormone is bound to thyroid-binding globulin (TBG) and testosterone is bound to sex hormone-binding globulin (SHBG). A very small percentage of cortisol is free and unbound, while the remaining is in transition.
The human body produces cortisol first, and then different glands can keep it as cortisol or convert it into cortisone, which is biologically inactive, through the enzyme 11-beta-hydroxysteroiddehydrogenase (11bHSD). Cortisol is then metabolized into 5a-tetrahydrocortisol (5a-THF) and 5b-tetrahydrocortisol (5b-THF) and cortisone is metabolized into 5b-tetrahydrocortisone (5b-THE).
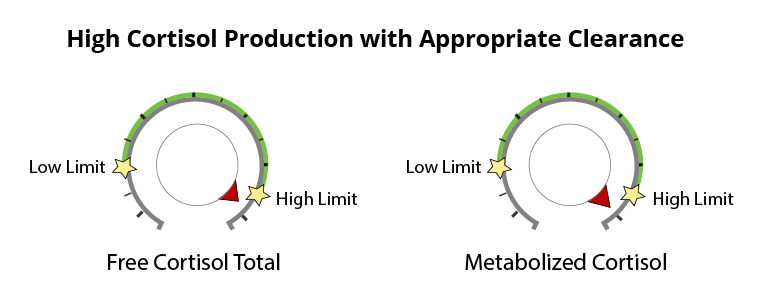
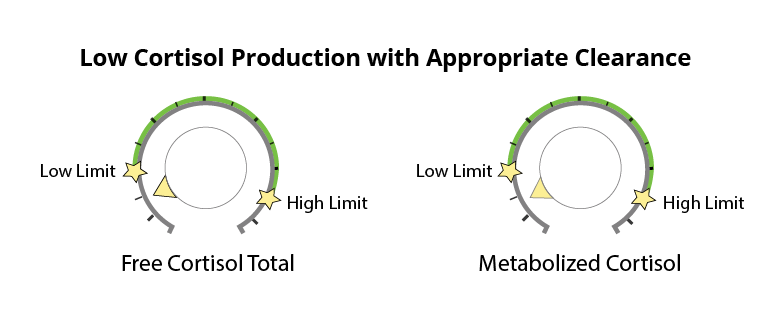
Since all production and output originally started as cortisol, the cortisone metabolites are added to the cortisol metabolites when evaluating the “total metabolized cortisol”. It essentially reflects how much cortisol was made in the body and has been processed out through the liver, into the kidney, and onto the DUTCH Test. See below for two examples of DUTCH Test results showing appropriate cortisol clearance.
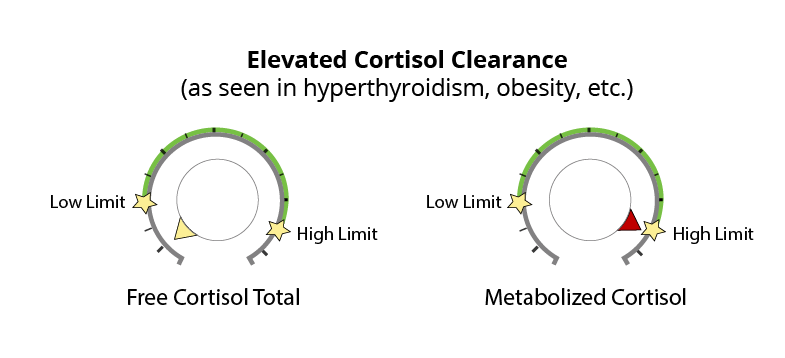
Elevated Cortisol Clearance
The amount of cortisol produced and the amount of free cortisol available can be different in some scenarios. Measuring both gives insight into the rate of cortisol clearance and metabolism. For example, higher levels of metabolized cortisol (compared to free cortisol) are often seen in obesity where adipose tissue is likely pulling cortisol from its binding protein and allowing for metabolism and clearance. The adrenal gland must keep up with cortisol sequestering and excretion, so cortisol production is often quite high (as seen in the levels of metabolized cortisol) even though free cortisol does not correlate positively with adipose tissue or BMI.
This insight may be helpful for those looking to lose belly fat and suspect that cortisol and stress are major factors. These patients are often misdiagnosed as having low cortisol production when only free cortisol is measured. Increased cortisol clearance may also be seen in hyperthyroidism and is suspected to be part of the chronic fatigue story as well.
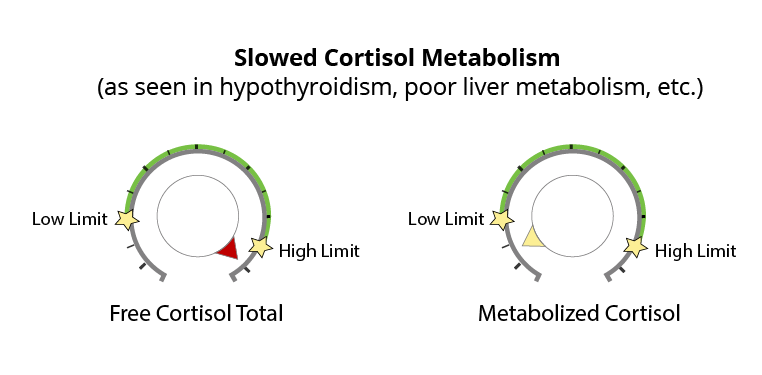
Slowed Cortisol Metabolism
In patients with low thyroid, the opposite pattern is often seen. When the thyroid slows down or in cases of peripheral hypothyroidism where free T3 cannot get into the cells, the clearance (or metabolism) of cortisol through the liver slows down. As a result, free cortisol starts to increase and may show up elevated on the DUTCH Test.
Metabolized and Free Cortisol Give the Whole Picture
The metabolized cortisol and free cortisol markers are important to use both together and separately to tell a more complete story about the patient. Metabolized cortisol answers the question of how much cortisol is made in total and cleared through the liver. Whereas free-cortisol results tell how much cortisol is free to bind to receptors and allow for assessment of the circadian rhythm. The metabolites of cortisol also give insight into the relative activity of 11b-HSD types I and II, which control the activation and inactivation (to cortisone) of cortisol.
Having the most comprehensive testing available with the DUTCH Test allows for a more complete look at the overall HPA axis picture. This in turn leads to better treatment and clinical outcomes.
References
- Abraham, S. B., Rubino, D., Sinaii, N., Ramsey, S., & Nieman, L. K. (2013). Cortisol, obesity and the metabolic syndrome: A cross-sectional study of obese subjects and review of the literature. Obesity (Silver Spring),21(1), 1-24. doi:10.1002/oby.20083
- Dhillo WS, Kong WM, Le Roux CW, Alaghband-Zadeh J, Jones J, Carter G, Mendoza N, Meeran K and O’Shea D. Cortisol-binding globulin is important in the interpretation of dynamic tests of the hypothalamic-pituitary-adrenal axis. Euro J Endo.2002;146
- Hoshiro, M., Ohno, Y., Masaki, H., Iwase, H., & Aoki, N. (2006). Comprehensive Study of Urinary Cortisol Metabolites in Hyperthyroid and Hypothyroid Patients. Clinical Endocrinology, 64, 37-45. doi:10.1111/j.1365-2265.2005.02412.x
- Taniyama, M., Honma, K., & Ban, Y. (1993). Urinary Cortisol Metabolites in the Assessment of peripheral Thyroid Hormone Action for Diagnosis of Resistance to Thyroid Hormone. Thyroid, 3, 229-233.
- Tomlinson, J. W., Finney, J., Hughes, B. A., Hughes, S. V., & Stewart, P. M. (June 2008). Reducing Glucocorticoid Production Rate, Decreased 5alpha-Reductase Activity, and Adipose Tissue Insulin Sensitization After Weight Loss. Diabetes,57, 1536-1543.